Хвороби серця є основною причиною смертності в усьому світі, а наявність сімейної схильності до цього захворювання може значно підвищити ризик.
Але що, якби існував спосіб зменшити цей спадковий ризик за допомогою простих змін у раціоні?
Революційне дослідження пролило світло на потенціал омега-3 жирних кислот, які містяться в жирній рибі, для протидії підвищеному ризику серцевих захворювань, пов’язаному з сімейною історією.

Розуміння ролі сімейної історії
Хвороби серця залишаються провідною причиною смерті у всьому світі, а наявність сімейного анамнезу серцево-судинних захворювань (ССЗ) наражає людей на ще більший ризик.
Потенціал дієтичних втручань
Але нове дослідження припускає, що споживання більшої кількості омега-3 жирних кислот, які містяться в жирній рибі, такій як лосось, сардини та скумбрія, може допомогти протидіяти цьому підвищеному генетичному ризику.
У дослідженні, опублікованому в журналі Circulation, проаналізовано дані 15 спостережних досліджень у 10 країнах, в яких взяли участь майже 41 000 дорослих людей без наявних серцевих захворювань. Отримані дані проливають світло на те, як дієта може взаємодіяти з генетичними факторами і впливати на здоров’я серця.

Клінічне дослідження: Методологія та результати
Учасники та збір даних
Дослідники вимірювали рівні різних поліненасичених жирних кислот (ПНЖК) у крові та тканинах учасників як маркери їхнього харчового раціону.
Аналіз рівнів ПНЖК та сімейного анамнезу
ПНЖК – це незамінні жири, які організм не може виробляти самостійно, тому вони повинні надходити з їжею.
Дослідження було зосереджено на трьох основних типах:
Типи досліджуваних ПНЖК
- ейкозапентаєнова кислота (ЕПК) та докозагексаєнова кислота (ДГК), в основному міститься в жирній рибі
- Альфа-ліноленова кислота (ALA), що міститься в рослинних джерелах, таких як лляне насіння, насіння чіа та волоські горіхи
- Лінолева кислота (ЛК), поширена в рослинних оліях, горіхах та насінні.
Учасники були віднесені до категорії з низьким рівнем споживання, якщо їх рівень ПНЖК знаходився в нижніх 25%.
Сімейний анамнез визначався як наявність принаймні одного родича першого ступеня спорідненості (батька або брата чи сестри), який пережив інфаркт або інсульт.
Виявлено значну взаємодію
Дослідження виявило значний взаємозв’язок між низьким рівнем ЕПК/ДГК та сімейним анамнезом. А саме:
- Особи з низьким рівнем ЕПК/ДГК та обтяженим сімейним анамнезом мали на 41% вищий ризик розвитку серцево-судинних захворювань порівняно з тими, хто не мав жодного з цих факторів ризику.
- Лише обтяжений сімейний анамнез підвищував ризик на 25%, тоді як низький рівень ЕПК/ДГК сам по собі суттєво не підвищував ризик.
- Не було виявлено жодних значущих взаємодій для АЛК або ЛПНЩ в сімейному анамнезі.
“Це дослідження свідчить про те, що люди з сімейною історією серцево-судинних захворювань можуть отримати ще більше користі від рекомендацій споживати їжу, багату на ЕПК і ДГК”, – зазначила провідний автор дослідження доктор Федеріка Лагуцці (Federica Laguzzi).

Інтерпретація результатів: Що це означає для вас
Взаємодія генів і дієти
Результати вказують на те, що підвищений ризик серцево-судинних захворювань, зумовлений сімейною історією, може бути посилений дієтою з низьким вмістом омега-3, що містяться в рибі.
Іншими словами, генетична схильність і харчові звички можуть взаємодіяти, формуючи здоров’я серцево-судинної системи.
Хоча ви не можете змінити свої гени, це дослідження припускає, що ви можете певною мірою модифікувати їх вплив за допомогою харчування.
Чинні рекомендації вже наголошують на споживанні риби як частині здорової для серця дієти.
Але це дослідження припускає, що ті, хто має сімейний анамнез серцевих захворювань, можуть отримати додаткову користь від забезпечення адекватного споживання омега-3.
“Хоча сімейний анамнез ССЗ є немодифікованим фактором ризику ССЗ, існує потенціал для обмеження його несприятливих наслідків”, – пишуть автори.
Вони зазначили, що, незважаючи на профілактичні зусилля, серцево-судинні захворювання залишаються основною причиною смертності, тому визначення груп високого ризику для проведення цілеспрямованих втручань має вирішальне значення.
Поставимо результати в контекст
Попередні дослідження показали позитивний зв’язок між омега-3 з риби та здоров’ям серця, хоча результати клінічних випробувань були неоднозначними.
Менш послідовні результати були отримані для ПНЖК рослинного походження, таких як ALA і LA, хоча останні дані, схоже, підтверджують їхню захисну роль.
У всьому світі споживання ПНЖК, як правило, нижче, ніж зазвичай рекомендується на рівні 5-11% від загального споживання енергії.
Автори відзначили, що в жодному з попередніх досліджень біомаркери ПНЖК не вивчалися в поєднанні з даними сімейного анамнезу для оцінки взаємозв’язків.
Велика, різноманітна вибірка та використання об’єктивних біомаркерів у цьому дослідженні підкріплюють висновки. Однак спостережний дизайн означає, що воно не може довести причинно-наслідковий зв’язок.
Щоб підтвердити, чи може збільшення споживання риби зменшити надмірний ризик серцево-судинних захворювань, пов’язаний із сімейною історією, потрібні рандомізовані контрольовані дослідження.

Загальна картина: Харчування та здоров’я серця
Сучасні дієтичні настанови та рекомендації
Таким чином, аналіз об’єднаних даних виявив значний взаємозв’язок між низьким вмістом омега-3 в раціоні харчування та обтяженою спадковістю щодо ризику серцево-судинних захворювань.
Хоча необхідні додаткові дослідження, отримані результати підкреслюють важливість здорового харчування, особливо для тих, хто має генетичну схильність.
Важливість персоналізованого харчування
Якщо у вашій родині є серцеві захворювання, у вас може з’явитися додатковий стимул включити в свій раціон більше жирної риби. Не любите рибу? Приймайте якісну добавку Омега 3, таку як Zest Omega або Smart Omega.
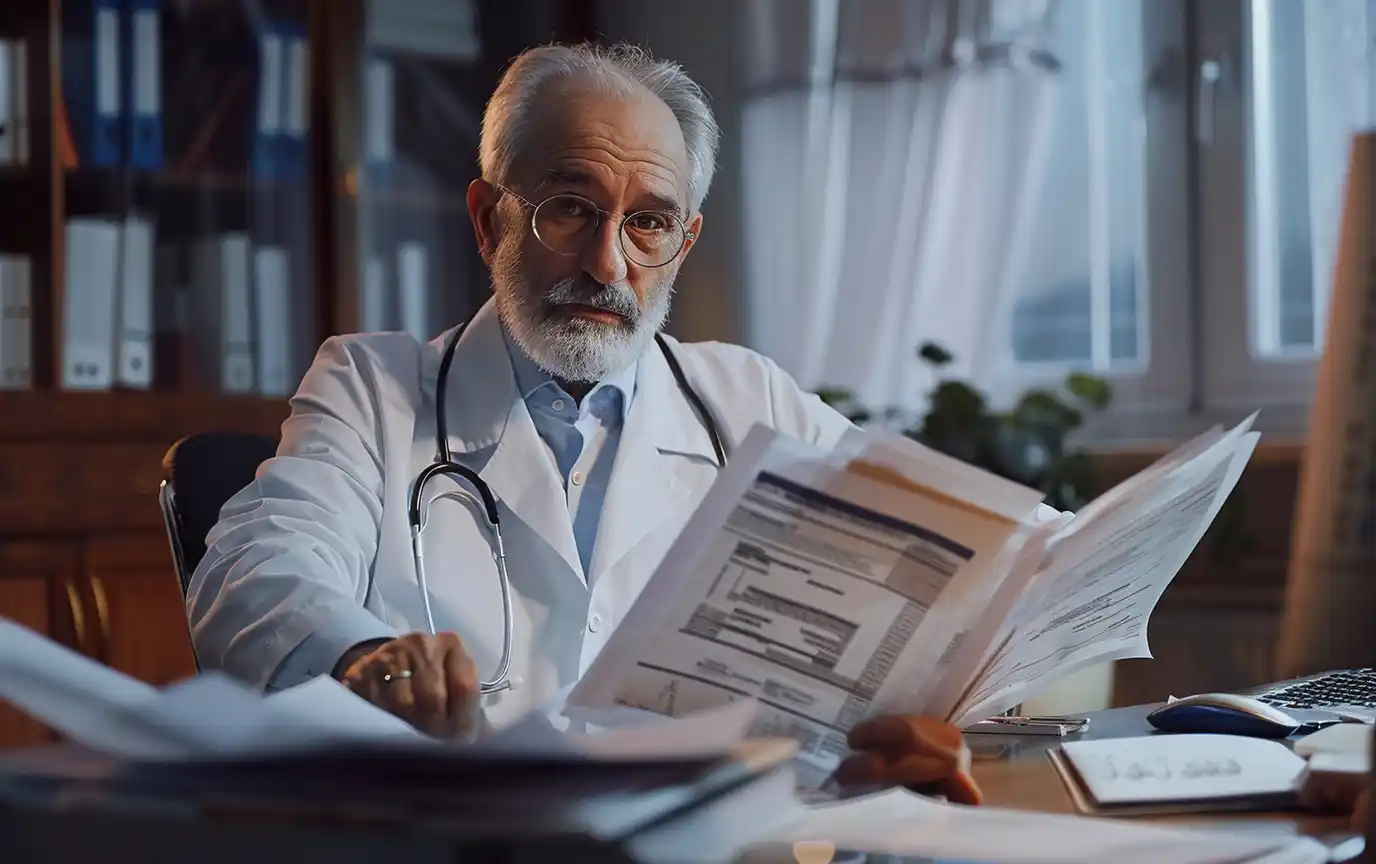
Робота з медичними працівниками
Поговоріть зі своїм лікарем або зареєстрованим дієтологом про ваші індивідуальні ризики та харчові потреби.
Навіть невеликі зміни, такі як вживання риби двічі на тиждень, можуть мати значення для здоров’я серця в довгостроковій перспективі.
Як підсумували автори дослідження:
“Цей новий результат може свідчити про необхідність підкреслити користь споживання жирної риби для осіб із сімейним анамнезом ССЗ”.