Understanding Lactose Intolerance: The Basics
What is Lactose Intolerance?
Lactose intolerance is a common digestive disorder that affects a significant portion of the global population. It’s characterized by the body’s inability to properly digest lactose, which is the primary sugar found in milk and dairy products. This condition occurs when there’s a deficiency of lactase, the enzyme responsible for breaking down lactose.
To understand lactose intolerance better, it’s important to break it down further:
- Lactose: This is a disaccharide sugar composed of glucose and galactose. It’s naturally present in milk and dairy products from mammals, including cows, goats, and humans.
- Lactase: This is an enzyme produced by cells lining the small intestine. Its primary function is to break down lactose into its component parts: glucose and galactose.
- Lactase deficiency: This is the root cause of lactose intolerance. When the body doesn’t produce enough lactase, lactose can’t be properly digested.
The Digestive Process and Lactose
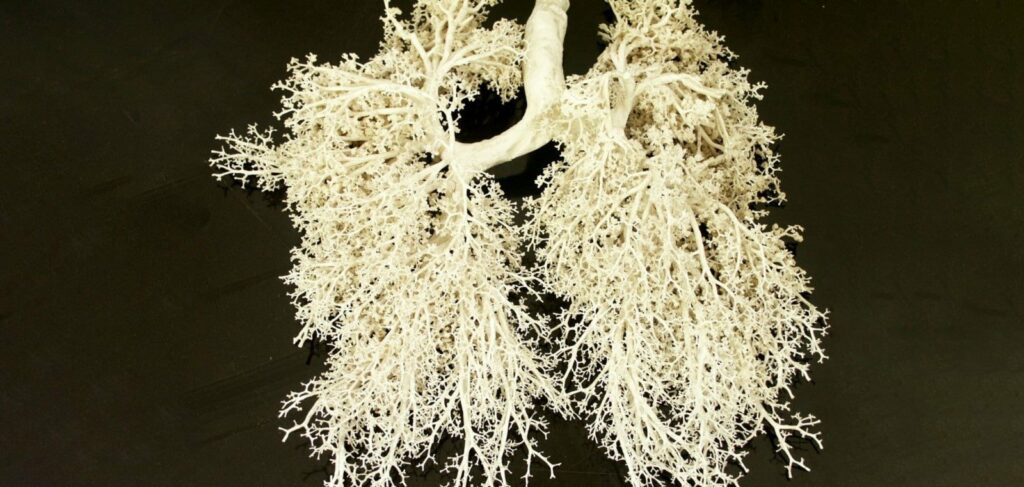
To fully grasp how lactose intolerance affects the body, it’s crucial to understand the normal digestive process for lactose:
Normal lactose digestion:
- When a person consumes milk or dairy products, the lactose travels through the stomach and into the small intestine.
- In the small intestine, lactase enzymes break down the lactose into glucose and galactose.
- These simple sugars are then absorbed through the intestinal wall into the bloodstream, where they can be used for energy.
Lactose intolerance:
- In individuals with lactose intolerance, there isn’t enough lactase to break down all the lactose consumed.
- The undigested lactose continues to travel through the digestive system to the large intestine (colon).
- In the colon, bacteria ferment the undigested lactose, producing gases and other byproducts.
- This fermentation process leads to the symptoms associated with lactose intolerance, such as bloating, gas, abdominal cramps, and diarrhea.
It’s important to note that lactose intolerance is not an allergy. Milk allergies involve the immune system, while lactose intolerance is a problem with digestion.
The severity of lactose intolerance can vary greatly among individuals, with some people able to tolerate small amounts of dairy while others need to avoid it completely.
The Science Behind Lactose Intolerance
What Happens When Lactose Isn’t Digested?
When lactase is insufficient or absent, undigested lactose moves to the large intestine. Here, it undergoes fermentation by gut bacteria, producing various byproducts:
- Fatty acids
- Gases: carbon dioxide, hydrogen, and methane
This fermentation process leads to the characteristic symptoms of lactose intolerance:
- Flatulence
- Abdominal rumbling
- Bloating
- Diarrhea (due to increased osmotic pressure causing water influx into the intestine)
- Abdominal pain and cramps
- Occasionally, nausea and vomiting
Lactose Intolerance in Infants
In babies, lactose intolerance manifests differently:
- Colic
- Bloating
- General irritability, especially after feeding
- Frequent, foamy stools with a sour odor
Timing and Severity of Symptoms
Symptoms typically develop within a few hours of consuming lactose-containing foods and can persist for 2-3 days. The severity varies based on:
- Amount of lactose consumed
- Individual tolerance levels
For instance, some individuals might tolerate a small glass of milk, while others experience discomfort from just a splash of milk in their coffee.
Types of Lactose Intolerance: Not All Are Created Equal
Understanding the different types of lactose intolerance is crucial for proper diagnosis and management.
Primary Constitutional Lactose Intolerance
This is the most common form of lactose intolerance, also known as adult-type hypolactasia or lactase non-persistence.
Cause: Natural decrease in lactase production with age
Primary lactose intolerance is caused by a genetically programmed gradual reduction in lactase production. This decrease is a normal biological process in most mammals, including humans.
After weaning, when milk is no longer the primary source of nutrition, the body naturally reduces lactase production.
Onset: Usually after age 2, but symptoms may not be noticeable until 20-40 years old
While the decrease in lactase production typically begins after age 2, the onset of noticeable symptoms can be quite variable:
- Gradual onset: The reduction in lactase is usually gradual, allowing the body to adapt slowly.
- Delayed symptom recognition: Many people may not recognize symptoms until early adulthood (20-40 years old) when dairy consumption patterns change or increase.
- Symptom variability: The severity and timing of symptoms can vary greatly among individuals.
Evolutionary aspect: About 10,000 years ago, a genetic mutation emerged allowing lactase persistence into adulthood
This evolutionary development is fascinating:
- Agricultural revolution: The mutation coincided with the advent of dairy farming, providing a survival advantage to those who could digest milk into adulthood.
- Positive selection: The ability to digest lactose as an adult (lactase persistence) spread rapidly in populations that practiced dairying.
- Genetic variation: The mutation affects the regulation of the lactase gene (LCT), not the gene itself.
Ethnic variations:
The prevalence of lactose intolerance varies significantly among different ethnic groups:
High prevalence (80-90%) in East Asia, Southern Africa, and South America:
- East Asia: Countries like China, Japan, and Korea have very high rates of lactose intolerance.
- Southern Africa: Many indigenous African populations have high lactose intolerance rates.
- South America: Native populations in countries like Peru and Bolivia show high prevalence.
Low prevalence (5-15%) in Eastern and Northern Europe, including Russian and Ukraine:
- Dairying history: These regions have a long history of cattle herding and dairy consumption.
- Genetic adaptation: The lactase persistence mutation is more common in these populations.
- Cultural factors: Dairy products have been a significant part of the diet for thousands of years.
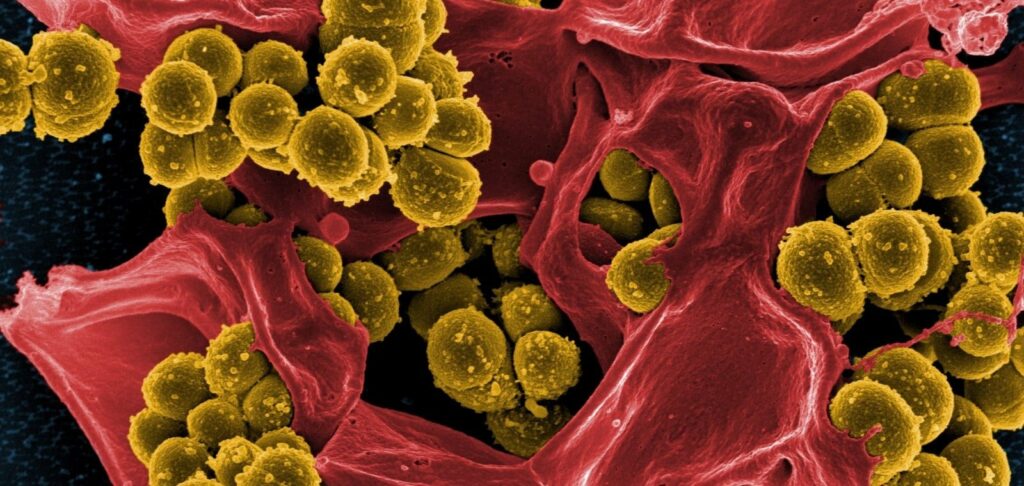
Secondary Lactose Intolerance
A temporary condition where lactase production is reduced due to damage to the small intestine.
Unlike primary lactose intolerance, this form can be reversible once the underlying condition is treated and the intestinal lining heals.
- Cause: Damage to the small intestine due to various conditions
- Common triggers:
- Acute gastroenteritis
- Celiac disease
- Crohn’s disease
- Ulcerative colitis
- Irritable bowel syndrome (IBS)
- Parasitic infections
- Antibiotic-induced dysbiosis
- Nature: Usually reversible with treatment of the underlying condition
- Prevalence: Most common form in infants and young children
Transient Lactose Intolerance
A temporary inability to digest lactose, typically in infants and young children.
Differs from primary/secondary intolerance due to its short-term nature and complete resolution.
- Affected group: Primarily premature infants
- Cause: Underdeveloped small intestine functions in babies born before 37 weeks gestation
- Duration: Typically short-lived and resolves quickly
Congenital Lactose Intolerance
- Type: Rare genetic disorder
- Characteristic: Inability to digest lactose from birth, including breast milk
- Inheritance: Autosomal recessive (both parents must carry the mutation)
- Historical context: Previously fatal for infants
- Modern management: Use of soy-based formula
Differential Diagnosis: Conditions That Mimic Lactose Intolerance
It’s crucial to distinguish lactose intolerance from other conditions with similar symptoms:
Irritable Bowel Syndrome (IBS)
IBS is a common functional gastrointestinal disorder characterized by recurrent abdominal pain and changes in bowel habits.
It’s a chronic condition that affects the large intestine, causing discomfort and altering bowel function without visible signs of damage or disease in the digestive tract.
- Cause: Unknown, possibly related to gut motility issues or oversensitive intestinal nerves
- Symptoms: Stomach cramps, bloating, diarrhea, and constipation
- Key difference: Symptoms persist even when dairy is eliminated from the diet
Milk Allergy
- Mechanism: Immune system reaction to cow’s milk proteins
- Symptoms: Skin rashes, itching, wheezing, and breathing difficulties
- Distinguishing factor: Reactions occur with even minimal milk consumption, unlike lactose intolerance where small amounts may be tolerated
7 Methods to Diagnose Lactose Intolerance: From Simple to Complex
Accurate diagnosis is key to proper management. Here are the various methods used to identify lactose intolerance:
Food and Symptom Diary
- Method: Keep a detailed log of food intake and associated symptoms for several weeks
- Benefit: Simple, non-invasive, and can be done at home
Elimination Diet
- Approach: Completely avoid dairy products for a period to observe symptom improvement
- Duration: Typically 2-4 weeks
Fecal Carbohydrate Analysis
- Primarily for: Young children
- What it measures: Content of reducing carbohydrates (glucose, galactose, lactose, fructose, maltose) in feces
- Significance: Elevated levels indicate sugar breakdown and absorption issues
Hydrogen Breath Test
- Process:
- Measure baseline hydrogen in exhaled air
- Drink a standard lactose solution
- Measure hydrogen levels again after a set time
- Positive result: Sharp increase in hydrogen, indicating bacterial fermentation of undigested lactose
Lactose Tolerance Test
- Method: Monitor blood glucose levels after consuming lactose
- Normal response: Quick rise in blood glucose
- Lactose intolerance indicator: Slow or no rise in blood glucose
Genetic Testing
- Target: MCM6 lactase gene polymorphism
- Usefulness: Identifies genetic predisposition to lactose intolerance
Small Intestine Biopsy
- When used: Rare cases requiring differentiation from other conditions (e.g., celiac disease)
- Procedure: Endoscopic sampling of small intestine mucosa
- Analysis: Test sample for lactase content
Managing Lactose Intolerance: Dietary Strategies and Beyond
While lactose intolerance doesn’t cause permanent damage to the gastrointestinal tract, managing symptoms is crucial for quality of life. Here are some effective strategies:
Dietary Modifications
Fermented dairy products
Many people with lactose intolerance can tolerate fermented dairy products for several reasons:
Reduced lactose content: During fermentation, bacteria consume much of the lactose in milk, converting it into lactic acid. This process significantly reduces the amount of lactose present in the final product.
Presence of live cultures: Fermented dairy products often contain live bacteria (probiotics) that can help break down remaining lactose in the gut.
Slower digestion: The thicker consistency of many fermented dairy products (like yogurt) slows down digestion, giving the body more time to process any remaining lactose.
Lactase production: Some fermenting bacteria produce small amounts of lactase, the enzyme needed to digest lactose.
Improved digestibility: The fermentation process partially breaks down milk proteins, making them easier to digest overall.
These factors combine to make fermented dairy products like yogurt, kefir, and certain cheeses more tolerable for many individuals with lactose intolerance, allowing them to enjoy some dairy in their diet without experiencing severe symptoms.
Sweet dairy products:
Sweet dairy products, such as ice cream and condensed milk, are often better tolerated by people with lactose intolerance due to the presence of alpha-glucosidase.
May seem strange, but here’s why:
Alpha-glucosidase role: This enzyme helps break down complex sugars into simpler forms.
Interaction with lactose: In sweet dairy products, alpha-glucosidase can partially break down lactose, making it easier to digest.
Sugar content effect: The high sugar content in these products can slow gastric emptying, allowing more time for lactose digestion.
Dilution effect: In ice cream, the fat content can dilute the lactose concentration, potentially reducing symptoms.
Processing impact: The processing of condensed milk may alter lactose structure slightly, potentially improving tolerability.
This combination of factors contributes to the improved tolerability of sweet dairy products like ice cream and condensed milk for many people with lactose intolerance, although individual responses may vary.
Raw milk is often better tolerated than processed milk, but why?
Natural enzymes: Raw milk contains the enzyme lactase, which is naturally present in small amounts. This lactase can help break down some of the milk’s lactose.
Beneficial bacteria: Raw milk contains live probiotic bacteria that may aid in lactose digestion in the gut.
Intact proteins: The proteins in raw milk are unaltered, potentially making them easier to digest for some people.
Bioactive components: Raw milk contains various bioactive substances that may support digestion and are often destroyed or altered during pasteurization.
Fat globule structure: The natural fat globule membrane in raw milk may slow lactose absorption, reducing symptoms.
Individual variability: Tolerance can vary significantly among individuals.
Limited scientific evidence: While anecdotal reports exist, scientific evidence supporting better tolerance of raw milk is limited.
These factors contribute to why some people with lactose intolerance report better tolerance of raw milk.
Enzyme Supplements
- Option: Lactase enzyme supplements (for example, Enzybar or Kuchikoo)
- Usage: Taken with dairy-containing meals
- Dosage: Adjusted based on individual needs and lactose content of foods
Gradual Adaptation
- Method: Regular consumption of small amounts of dairy products
- Benefit: Can promote adaptation of colon bacteria, potentially reducing intolerance over time
Reading Food Labels
For individuals with lactose intolerance, reading food labels is crucial for managing their condition and avoiding unexpected digestive issues.
It’s particularly important for identifying hidden sources of lactose in processed foods, as lactose can be present in many products that aren’t obvious dairy items.
Why It’s Important:
- Avoid symptoms: Careful label reading helps prevent accidental lactose consumption and subsequent digestive discomfort.
- Expand food choices: Understanding labels allows for a wider variety of safe food options.
- Nutritional balance: It helps in maintaining a balanced diet while avoiding lactose.
Common Hidden Sources of Lactose:
Whey:
- What it is: A byproduct of cheese production, rich in protein.
- Where it’s found: Protein powders, baked goods, processed meats.
- Why it’s used: For its nutritional value and as a binding agent.
Milk Solids:
- What they are: The dried powder left after all moisture is removed from milk.
- Where they’re found: Baked goods, soups, sauces, coffee creamers.
- Why they’re used: To add flavor, texture, and nutritional value.
Non-Fat Milk Powder:
- What it is: Pasteurized skim milk with water removed.
- Where it’s found: Baked goods, instant soups, coffee mixes, some medications.
- Why it’s used: As a thickener, for flavor, and to increase nutritional content.
Other Terms to Look Out For:
- Casein
- Lactose
- Lactoglobulin
- Lactalbumin
- Recaldent (in some dental products)
Tips for Effective Label Reading:
- Check ingredient lists thoroughly, not just the front of the package.
- Be aware that “non-dairy” doesn’t always mean lactose-free.
- Look for “contains milk” statements, which are required on labels for common allergens.
Nutritional Considerations
- Calcium intake: Ensure adequate calcium from non-dairy sources or supplements
- Vitamin D: May need supplementation if avoiding dairy products
Interesting Facts
- Sucrose effect: Adding 1-5% sucrose to dairy products can increase lactose tolerance by 48-96%
- Raw milk tolerance: Some individuals with lactose intolerance can drink raw milk due to its natural enzymes
- Ethnic variations: Lactose intolerance rates vary significantly across ethnicities, reflecting evolutionary adaptations to dairy consumption
Lactose Intolerance in Perspective
Lactose intolerance, while common in many parts of the world, is neither a universal condition nor a severe health threat when properly managed.
Understanding your body’s tolerance levels, being aware of lactose content in foods, and employing appropriate dietary strategies can help individuals with lactose intolerance lead comfortable, healthy lives without completely eliminating dairy from their diets.