Most people tolerate grains quite well, but for the 0.5-1% of the world’s population diagnosed with celiac disease, eating some of them is deadly.
Celiac disease is an autoimmune disorder
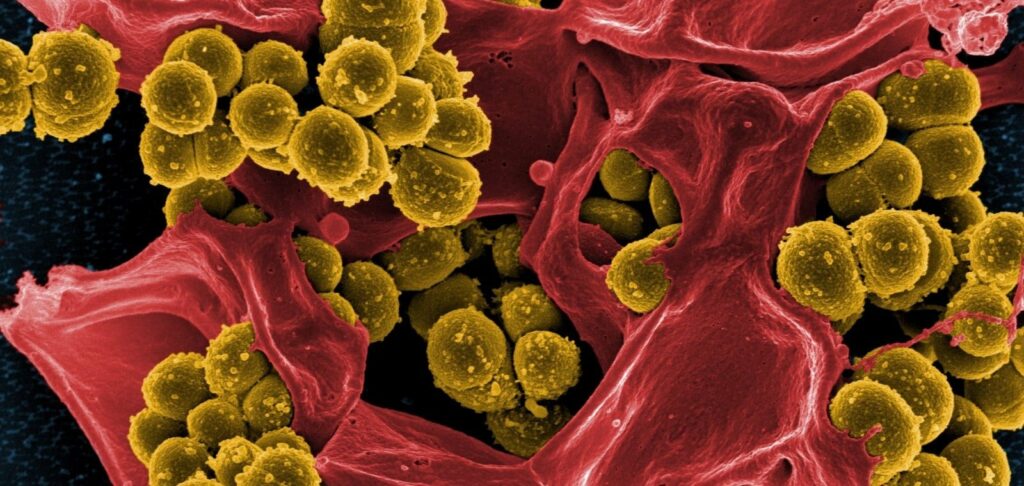
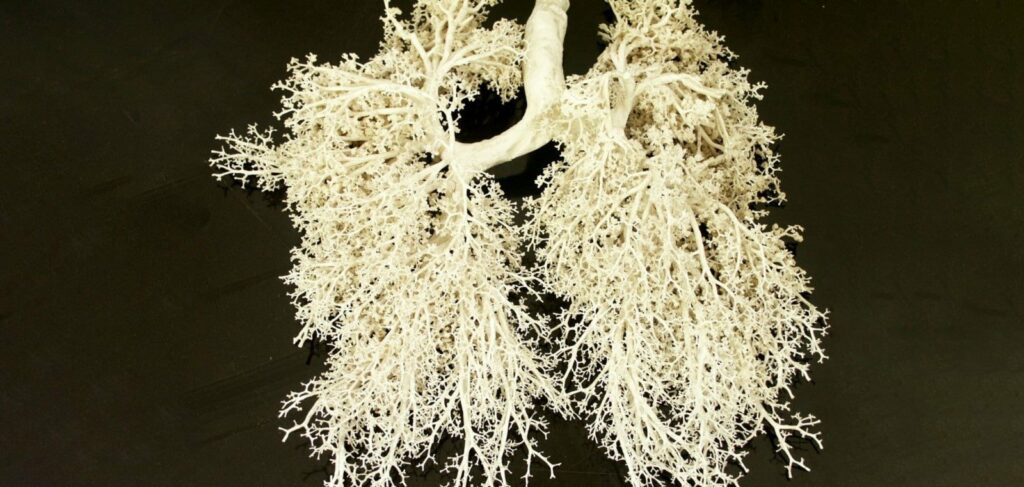
Some cereals contain two types of simple proteins, prolamins and glutelins. When they interact, gluten is formed. When wheat flour is mixed with water, it is what creates the elastic, sticky and gummy consistency of dough, which is why it is often called gluten. Some people’s bodies do not react properly to gluten. This is how celiac disease, an autoimmune disorder in which the immune system attacks gluten as a foreign invader, and with it, the villi that cover the small intestine. As a result, the intestinal mucosa becomes inflamed, the villi eventually shorten and atrophy. This leads to serious impairment of the absorption of minerals and nutrients, which is fraught with a significant deterioration of health, and in severe cases – even death.
The symptoms of celiac disease usually appear in infancy, with the introduction of the first complementary food containing cereals. However, celiac disease can occur in adulthood if there is a genetic predisposition. Autoimmune diseases (e.g. type I diabetes, rheumatoid arthritis, Hashimoto’s thyroiditis, etc.); genetic pathologies, in particular Down’s syndrome or Turner’s syndrome; heredity – if there is at least one relative suffering from celiac disease, the probability of getting the disease increases 10 times.
Symptoms and effects of celiac disease
Celiac disease causes intestinal problems (bloating, diarrhea), decreased appetite, poor weight gain, restlessness and irritability in children. Over time, celiac disease causes damage to tooth enamel, anemia, delayed development, growth and puberty.
In adults, the symptoms of this disease are more varied. They can range from mild to severe and can also change over time. Celiac disease has been known to occur without obvious signs. The patient may have only general malaise, chronic fatigue, anemia and abdominal discomfort. But it happens that in addition to GI disorders (diarrhea and flatulence), gluten intolerance entails a whole bunch of unpleasant and dangerous symptoms:
- bone and joint pain, muscle weakness and cramps;
- depression, irritability, weakness and fatigue;
- nosebleeds, blood in feces or urine;
- fluid retention in the body;
- constant hunger;
- iron deficiency anemia, deficiency of vitamins B12, D and K;
- Dühring’s dermatitis herpetiformis, in which red bulging spots and blisters appear on the skin.
The severity of the disease usually depends on the amount of gluten consumed, the age at which the disease began, and the degree of damage to the small intestine. If a person with celiac disease continues to consume gluten, sooner or later he or she will develop various complications, such as coronary heart disease, osteoporosis, infertility, intestinal lymphoma, and so on.
In some cases, the body attacks not only the cells lining the mucosa of the small intestine, but also a part of the brain called the cerebellum, resulting in gluten ataxia. The symptoms of this condition start with minor neurological manifestations, such as tingling in the legs and feet, and build up very slowly. However, if gluten is not avoided in time, irreversible damage (atrophy) of the cerebellum may develop, causing problems with balance, general movement, coordination, fine motor skills and so on. Gluten ataxia is still poorly understood and its prevalence is difficult to calculate. Researchers believe that gluten may be the culprit in 23-41% of people with ataxia of unknown origin.
Similar signs of other ailments
Celiac disease is a very rare condition. According to statistics, it occurs in 0.5-1% of people. However, other diseases can cause symptoms similar to those of celiac disease. For example, another 1% of the world’s population suffers from wheat allergy, which can manifest itself with gastrointestinal symptoms, as well as respiratory and skin manifestations. It occurs most often in young children, but most of them outgrow it by school age.
In addition, quite a few people have neither allergic nor autoimmune reactions to gluten, but do not tolerate it well. Against the background of consuming products containing gluten, they suffer from diarrhea, abdominal pain and bloating, constant fatigue, depression. However, recently more and more experts say that all these unpleasant symptoms are caused not by gluten, but by other substances. The most likely “suspects” are short-chain carbohydrates (oligo-, di-, monosaccharides and polyols), which are not fully absorbed in the small intestine and cause increased gas. This conclusion is supported by numerous experiments in which people with gluten sensitivity were given a diet low in short-chain carbohydrates, after which their condition improved markedly. Then isolated gluten was added to their diet, which generally had no effect on their well-being. In addition, symptoms similar to celiac disease can occur in exocrine pancreatic insufficiency, Crohn’s disease, irritable bowel syndrome, and so on.
Difficulties of diagnosis and lifelong dieting
Because of the vague clinical picture and the variety and variability of symptoms, it is not easy to diagnose celiac disease. Statistics show that in some countries of the world up to 80% of people with gluten intolerance do not suspect that they are ill. At the same time, a significant number of self-diagnosed patients, on the contrary, are sure that they are gluten intolerant, although their diagnosis is usually not confirmed.
The first step in detecting celiac disease is a serologic blood test. Until a few years ago, tests for anti-reticulin antibodies (ARA), anti-gliadin antibodies (AGA) and anti-endomysial antibodies (EMA) were considered standard tests. However, ARA testing has proven to be insufficiently accurate for routine diagnostic use and is hardly used today. Instead, it is recommended that patients with suspected celiac disease be tested for antibodies against tissue transglutaminase (tTG) and disaminated gliadin peptides (DGP), as well as serum total IgA levels.
All of these tests should be taken in combination. Each of them is quite accurate and specific in people with classic symptoms and complete villous atrophy, but their sensitivity is reduced from 90% to 30% in minor lesions of the small intestinal mucosa.
If at least one of these tests is positive, the patient is scheduled for an intestinal biopsy, which remains the gold standard for diagnosing celiac disease. However, if clinical suspicion remains high, the doctor may also order this procedure if the serologic tests are negative.
The only effective therapy for celiac disease is to follow a strict gluten-free diet. Wheat, malt, barley and rye, as well as products containing them: cakes, cookies, pastries, pasta, beer, dumplings or dumplings, certain sweets, etc. should never be consumed. Please note that even safe products such as oats or peas may contain gluten due to the way they are produced.
With strict adherence to the diet, the symptoms of the disease disappear quite quickly. Damage to the intestine is eliminated within a few weeks and antibody levels return to normal within a few months after the elimination of gluten from the diet. However, repeated consumption of foods containing gluten can cause a relapse of the disease, so the diet must be adhered to permanently and for life.