

Lipase is a digestive enzyme responsible for breaking down fats into simpler compounds (fatty acids and glycerol) that can be digested in the intestine.
It is produced in the pancreas and partially in the stomach and intestine.
If lipase is deficient, fats are not fully digested, causing a feeling of heaviness, bloating, flatulence, diarrhea and, consequently, deficiency of fat-soluble vitamins (A, D, E, K).

When is lipase especially needed?
Lipase deficiency can be caused by:
- pancreatic enzyme deficiency (including chronic pancreatitis);
- liver and gallbladder disease;
- after a large fatty meal;
- absorption disorders (e.g., celiac disease, SIBP);
- with age – natural decrease in enzyme production.
In such cases, taking lipase in supplement form can help ease digestion and improve overall GI health.
Table 1. Symptoms associated with lipase deficiency
| Symptom | Possible cause |
|---|---|
| Heaviness and pain in the abdomen | Undigested fats |
| Greasy stool sheen | Statorea (fat in the feces). |
| Bloating, gas | Bacterial fermentation of fats |
| Dry skin | Deficiency of fat-soluble vitamins |
| Fatigue, weakness | Lack of energy from lipids |
How lipase works: a simple mechanism
- Fats from food enter the small intestine
- Lipase breaks down fats to fatty acids and glycerol
- Bile acids help emulsify fats
- Nutrients are absorbed into the bloodstream and used to provide energy for the body.
If lipase is insufficient, fats are passed around – literally, which not only reduces the nutritional value of the diet, but also stresses the liver, intestines, and even the skin (via systemic inflammation).

Lipase as a dietary supplement: indications and benefits
In the pharmacy, lipase can be found as part of complex enzyme preparations (e.g., pancreatin, multi-enzyme supplements).
It is important to choose preparations with acid-resistant coating, so that the enzyme will not be destroyed in the stomach.
Recommendations for lipase intake:
- after a large or fatty meal;
- in case of enzyme deficiency;
- in case of bloating and stool disturbance after eating fatty food;
- in case of liver and gallbladder diseases (in consultation with a doctor).
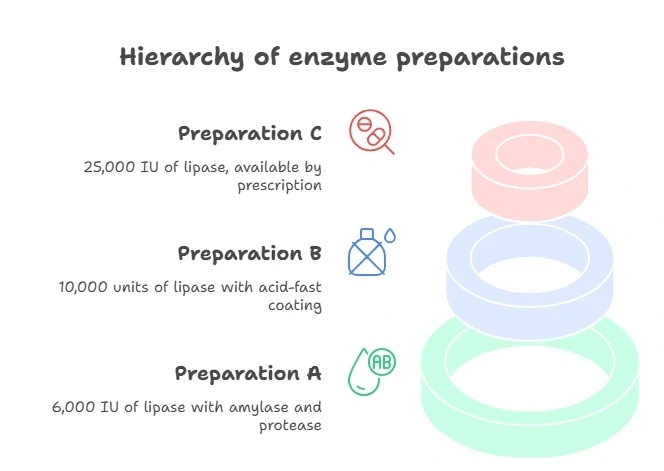
Table 2. Comparison of enzyme activity of popular additives
| Name of drug | Lipase content (units per dose) | Additionally |
|---|---|---|
| Preparation A | 6,000 IU | + amylase, protease |
| Preparation B | 10 000 IU | acid-proof shell |
| Preparation C | 25 000 IU | prescription drug |
UD – unit of enzyme action according to the international classification

Enzymes, liver and skin: unexpected links
Liver, lipids and skin: how is everything connected?
Many patients and even some physicians tend to think of skin manifestations such as shine, acne or irritations as a localized problem.
In reality, however, the skin is very sensitive to internal metabolic processes, especially the digestive system and the liver.
One of the key factors in this chain is the complete breakdown of fats.
Why does poor fat digestion harm the skin?
When lipase is deficient, fats are not digested but remain in the intestinal lumen
This causes bloating, diarrhea and impaired absorption of fat-soluble vitamins A, D, E and K.
These vitamins are critical for skin health – they regulate the sebaceous glands, participate in cell renewal, and have anti-inflammatory properties.
Fats that are not properly digested overload the liver
The liver has to compensate for the lack of enzymes, which increases the production of bile. In this case, its stagnation is possible – cholestasis.
This leads to impaired excretion of toxins, which directly affects the skin condition: rashes, dull complexion, itching.
Fat imbalance impairs the barrier function of the skin
The skin becomes more sensitive, prone to inflammation and irritation, and is less able to retain moisture.
This is especially noticeable in people with seborrheic dermatitis and acne – the skin becomes oily, but also dehydrated and inflamed.
What about systemic inflammation?
When fats are poorly digested, they can become “fuel” for pathogenic microflora in the gut.
Their fermentation process releases substances that increase inflammation, both in the gut and systemically.
It’s what’s called metabolic endotoxicosis.
Studies show that low-intensity chronic inflammation is associated with activation of skin immune cells and increased symptoms at:
- acne (increased sebum production + inflammation),
- rosacea (risk of redness and irritation),
- eczema and atopic dermatitis (deterioration of the skin barrier).
📚 См.: Jiang, Y. et al. (2018). Gut–skin axis: The role of intestinal microbiota in skin inflammation. Journal of Dermatological Science.
How does lipase help?
- Facilitates digestion of fats → reduces the burden on the liver and biliary system.
- Improves absorption of vitamins A, D, E, K → supports healthy skin and mucous membranes.
- Reduces the likelihood of dysbacteriosis and inflammation in the gut → skin receives fewer “alarm signals”.
- Indirectly reduces rashes, oiliness and skin irritation.
This is especially noticeable in patients with functional GI disorders (SIBP, enzyme deficiency, biliary dyskinesis) and chronic dermatoses, where lipase can be an important part of a comprehensive approach – along with diet, probiotics and topical therapy.
List of references
-
Martinsen, T.C. et al. (2005). The role of lipase in digestion. Scandinavian Journal of Gastroenterology.
-
Keller, J. et al. (2017). Functional testing in diseases of the exocrine pancreas: The end of an era? Pancreatology.
-
Krawczyk, M. et al. (2017). Link between digestive enzymes and cutaneous manifestations. Journal of Clinical Gastroenterology.




