The prevalence of secondary fungal infections is increasing, especially in patients with severe somatic diseases undergoing antibacterial, cytostatic, and immunosuppressive therapies. Today, pharmacies offer hundreds of brand-name antifungal medications to assist these patients.

Overview of Antifungal Medications
Antifungal drugs have been in use for nearly a century. The first successful use of potassium iodide for treating dermatophyte infections was reported in 1903.
Over the next 50 years, progress in developing antifungal agents was minimal until the introduction of nystatin in 1951. In 1956, studies evaluated the effectiveness of amphotericin B, another systemic drug.
In 1964, flucytosine began being used, and by the 1970s, second-generation antifungals, including imidazole derivatives (such as miconazole and ketoconazole), were introduced.
Ten years later, triazole compounds (itraconazole, fluconazole) and allylamines (terbinafine, naftifine) emerged as third-generation antifungals.
The most modern, fourth-generation drugs include liposomal forms of polyene antibiotics (amphotericin B and nystatin), new triazole derivatives (voriconazole, posaconazole, ravuconazole), and echinocandins (caspofungin).
Modern antifungal agents are available for all age groups—from newborns to the elderly—and come in a variety of forms.
Systemic mycoses are treated with intravenous solutions, tablets, capsules, dragees, and oral suspensions.
Topical treatments include ointments, creams, gels, sprays, powders, lotions, shampoos, solutions, antifungal nail lacquers, vaginal tablets, and suppositories.
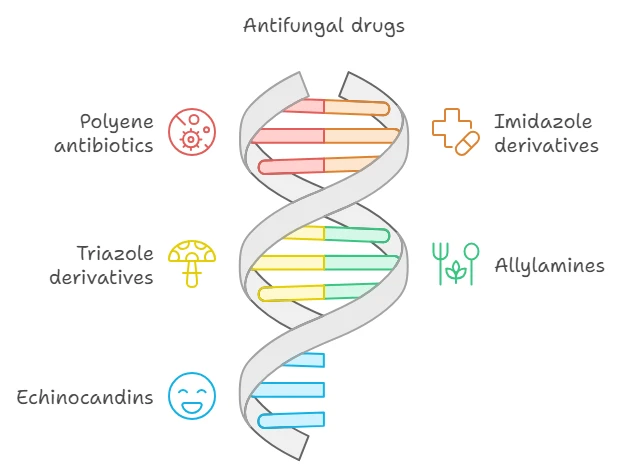
Classification of Antifungal Agents by Chemical Structure
- Polyene Antibiotics: Nystatin, levornidazole, natamycin, amphotericin B, micofepin.
- Imidazole Derivatives: Miconazole, ketoconazole, isoconazole, clotrimazole, econazole, tioconazole, bifonazole, oxiconazole, etc.
- Triazole Derivatives: Fluconazole, itraconazole, voriconazole, etc.
- Allylamines (N-methyl naphthalenes): Terbinafine, naftifine.
- Echinocandins: Caspofungin.
- Other Groups: Griseofulvin, amorolfine, ciclopirox, etc.

Systemic Antifungal Agents
Azole Antifungals
In clinical practice, azole antifungals are most commonly used for systemic mycoses.
Azoles are effective when taken orally or administered intravenously in patients with fungal infections caused by Candida spp., including generalized candidiasis in immunocompromised states, as well as mycoses caused by Cryptococcus neoformans, Microsporum spp., Blastomyces dermatitidis, Aspergillus, Coccidioides immitis, Histoplasma capsulatum, and Trichophyton spp.

Polyene Antibiotics
Polyene antibiotics are active against yeast-like fungi and some agents causing deep mycoses (Coccidioides, Histoplasma, Cryptococcus, Sporothrix), but their effectiveness is significantly lower against mold fungi and dermatophytes.
Besides their antifungal action, drugs in this group inhibit the activity of protozoa (amoebae, trichomonads, trypanosomes, leishmania) and also exhibit antiviral and anti-blastomycotic properties.
Mechanism of Action
Most antifungal agents work by disrupting metabolic processes in the fungal cell membrane, inhibiting reproduction and growth.
At high concentrations, both fungistatic (inhibiting growth) and fungicidal (killing the microorganism) effects are achieved.
Antifungal medications also possess immunomodulatory properties. Polyenes influence T and B lymphocytes of the immune system, enhance phagocyte activity, and stimulate bone marrow cell proliferation.
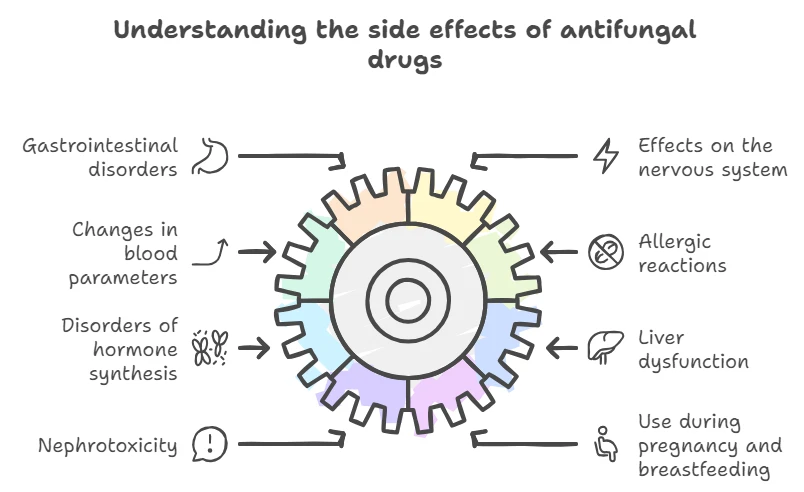
Side Effects of Systemic Antifungal Agents
Antifungal agents may cause gastrointestinal disturbances such as nausea, abdominal pain, diarrhea, and bloating. Nervous system side effects are rare but can include headaches and transient neuropathies.
Changes in peripheral blood counts (leukopenia, thrombocytopenia, hypokalemia), phlebitis from intravenous administration, and allergic reactions are possible.
Cases of disrupted endogenous steroid synthesis, frigidity, and impotence have been reported with azole use. Systemic administration can lead to liver dysfunction with elevated transaminases.
Due to the nephrotoxic effects of polyene antibiotics, intravenous use must be closely monitored for kidney function.
Azoles and systemic polyenes are not recommended during pregnancy and lactation. Natamycin may be used in pregnant and breastfeeding women, as well as in newborns.
New Antifungal Agents
Caspofungin
The first member of the new echinocandin class is caspofungin, which has a fundamentally different mechanism of action compared to other antifungals.
Caspofungin inhibits the synthesis of β-(1,3)-D-glucan, disrupting the fungal cell wall. Since mammalian cells do not contain β-(1,3)-D-glucan, caspofungin selectively targets fungi, resulting in good tolerability and few adverse reactions that typically do not require discontinuation of therapy.
It is fungicidal against Candida spp. strains and fungistatic against Aspergillus spp. Caspofungin is administered intravenously only.
Voriconazole
Voriconazole, a new triazole derivative, has a broader spectrum of activity and superior pharmacokinetic properties compared to its predecessor fluconazole.
Voriconazole inhibits the enzyme responsible for ergosterol production in fungal cell membranes more effectively.
It is active against all Candida and Aspergillus species, including strains resistant to fluconazole and itraconazole. Voriconazole also acts against Fusarium spp., Cryptococcus spp., Scedosporium apiospermum, and other fungi, including dermatophytes and endemic mycosis pathogens.
The drug penetrates the blood-brain barrier well, achieving high concentrations in cerebrospinal fluid, making it suitable for treating fungal meningitis.
Posaconazole
In 2006, the FDA approved posaconazole, a new antifungal agent available as an oral suspension.
It is active against Candida and Aspergillus species, including strains resistant to fluconazole, voriconazole, itraconazole, and amphotericin B. Posaconazole is considered a first-line treatment for oropharyngeal candidiasis in patients with severe disease and compromised immune systems, such as those with immunodeficiency following bone marrow transplantation or blood system cancers.
Research for new effective antifungals continues globally, with active studies on compounds such as corinexandin, fusacandin, sordarins, cyspentaquin, and azoxibacillin.

Emerging Antifungal Agents
Fosmanogepix
Fosmanogepix is a promising antifungal agent targeting the Gwt1 enzyme, crucial for fungal cell wall integrity.
It has shown effectiveness against a wide range of fungal pathogens, including multidrug-resistant strains.
Clinical trials have demonstrated its potential in treating candidemia and invasive mold infections with both intravenous and oral formulations.
Ibrexafungerp
Ibrexafungerp, a first-in-class triterpenoid antifungal, has been approved for vulvovaginal candidiasis and is under investigation for treating invasive fungal infections.
It demonstrates broad-spectrum activity, including against echinocandin- and azole-resistant strains.
Olorofim
Olorofim targets rare mold infections by inhibiting dihydroorotate dehydrogenase, a key enzyme in pyrimidine synthesis. It is effective against azole-resistant Aspergillus species and is currently in Phase 3 trials.
These emerging agents represent significant advancements in antifungal therapy, offering new mechanisms of action to combat resistant fungal infections.
Oral and Parenteral Antifungals
ATC Classification System: Dermatological Agents
- D01A A01 – Nystatin
- D01A A02 – Natamycin
- D01B A01 – Griseofulvin
- D01B A02 – Terbinafine
ATC Classification System: Systemic Antifungal Agents
- J02AA – Antifungal Antibiotics:
- J02AA A01 – Amphotericin B
- J02AA A02 – Gaciticin
- J02AB – Imidazole Derivatives:
- J02AB01 – Miconazole
- J02AB02 – Ketoconazole
- J02AC – Triazole Derivatives:
- J02AC01 – Fluconazole
- J02AC02 – Itraconazole
- J02AC03 – Voriconazole
- J02AC04 – Posaconazole
- J02AX – Other Systemic Antifungals:
- J02AX01 – Flucytosine
- J02AX04 – Caspofungin
- J02AX05 – Micafungin
- J02AX06 – Anidulafungin
- J02AX10 – Others
Treatment Considerations for Fungal Infections
Superficial and Nail Fungal Infections
Fungal infections of the feet, nails, scalp, and skin are the most common, with onychomycoses being predominant. For superficial nail plate infections, topical treatments may suffice.
Systemic therapy is indicated for onychomycoses affecting up to two-thirds of the nail depth, with moderate to severe hyperkeratosis, or when the infection involves nearly the entire nail even without significant thickening.
Widespread onychomycosis with deep nail involvement requires combination therapy using both topical and systemic antifungals.
Terbinafine and itraconazole are the drugs of choice for skin and nail mycoses, as well as fungal hair infections (such as trichophytosis and microsporia).
Amphotericin B and griseofulvin are used less frequently.
Candidiasis of the Digestive and Urogenital Tracts
Candidiasis is particularly common in the digestive and urogenital tracts.
Fungal infections of the gastrointestinal tract often lack a distinctive clinical picture, presenting as chronic gastritis, duodenitis, or enterocolitis, which complicates diagnosis.
For gastrointestinal candidiasis, the non-absorbable antifungal natamycin, which acts only within the digestive tract, is advisable.
Posaconazole is recommended by international specialists not only for treatment but also for the prevention of upper gastrointestinal candidiasis.
For urogenital candidiasis, short-term systemic antifungal therapy with fluconazole and other triazole derivatives is typically prescribed.
Acute Disseminated Candidiasis
Acute disseminated candidiasis is a serious condition that develops from hematogenous spread of Candida species, possibly during invasive procedures, manipulations, bone marrow, or organ transplants.
Clinically, this condition often presents with persistent or recurrent fever despite broad-spectrum antibiotic therapy. The mortality rate for candidemia is 40%, and for acute disseminated candidiasis (affecting multiple organs), it rises to 70–80%.
Effective treatments for candidiasis include amphotericin B, fluconazole, itraconazole, voriconazole, and caspofungin.
Itraconazole should not be used as initial therapy for invasive candidiasis due to the time required to achieve stable blood concentrations (1–2 weeks).
Candidal Meningitis
Candidal meningitis is treated with voriconazole, amphotericin B (or its liposomal forms), fluconazole, and flucytosine in combination with other antifungals.
Aspergillosis Infections
In recent years, there has been an increase in aspergillosis infections of the respiratory organs caused by various Aspergillus mold species.
These infections can masquerade as sinusitis, bronchial asthma, and chronic obstructive pulmonary disease.
Unfortunately, the frequency of invasive aspergillosis has also risen, with a mortality rate exceeding that of similar forms of candidiasis, reaching up to 87%.
Treatment for various forms of aspergillosis includes triazole derivatives (itraconazole, voriconazole), amphotericin B, and caspofungin.
Important Considerations in Antifungal Therapy
When treating patients with fungal infections, it is essential to consider:
- The severity of the disease
- The type of pathogen
- The condition of the affected target organ
- Side effects of antifungal agents
- Interactions with other medications
- The status of the liver and kidneys