What is Erythremia?
Another name for erythremia is true polycythemia, which comes from the Greek words “many”, “cell” and “blood”, which quite reflects the essence of the problem. The fact is that this disease is a benign tumor process of the hematopoietic system, associated with excessive myeloproliferation, ie, hyperplasia of the cellular elements of the bone marrow. As a result, they begin to produce too many red blood cells and platelets, which leads to an increase in the total mass of circulating blood (sometimes almost double), increasing its viscosity, slowing down the speed of blood flow, clogging small capillaries and increasing the risk of blood clots.
The disease is most often found in adult and elderly males. The average age of those affected ranges from 60 to 79 years. However, young people can also fall ill. In women, erythremia is one and a half times less common than in men, but often begins earlier and runs more complicated. It is known that there is a familial predisposition to true polycythemia, but the exact mode of inheritance is not yet clear.
How does the disease manifest itself?
The most common complaint in erythremia is severe itching in the hands or feet in about 40% of patients. It is usually intensified by contact with warm water, which is due to abnormal release of serotonin, histamine and prostaglandins. Due to the too slow movement of blood, as a result of which most of the hemoglobin has time to pass into the reduced form, the human skin acquires a reddish-cherry color, which is especially noticeable on its exposed parts: face, neck, hands, ankles and calves of the legs. Sometimes in erythremia, dilated veins located in the neck area are also visible, the conjunctivae and whites of the eyes turn red, and mucous membranes swell slightly.
A fairly common symptom of the disease is erythromelalgia, which is a burning pain in the tips of the fingers and toes and red or blue skin on these parts of the body. Erythromelalgia is caused by an increase in the number of platelets and their increased aggregation, causing tiny blood clots to form in small capillaries.
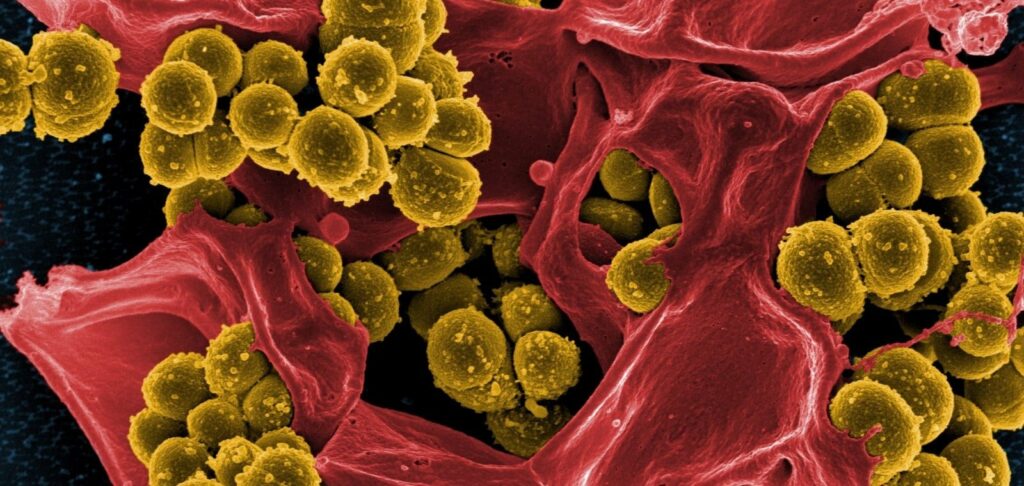
Approximately 20% of patients with polycythemia develop gouty arthritis, among other conditions. Another associated disease, which affects about 10-15% of patients with erythremia, is peptic ulcer disease of the stomach and duodenum. Thrombosis of small vessels leads to trophic disorders in the mucous membranes of these organs, which increases their susceptibility to damage by the bacterium H. pylori. As a compensatory reaction of the vascular bed to the increase in blood viscosity, blood pressure increases.
Non-specific symptoms of the disease may also include headaches, sometimes developing into excruciating migraines with visual disturbances. Many patients complain of pain in the heart area, in the bones, in the underbelly. They often experience dizziness, tinnitus, chronic fatigue, mood swings, decreased concentration and cognitive impairment.
The course of erythremia is usually divided into several stages
– First. Lasts for about 5 years from the onset of the disease, characterized by asymptomatic course or moderate manifestation of signs without any complications.
– Second. Develops within 5-15 years. The general blood test shows a high content of erythrocytes, platelets and leukocytes. Symptoms become more pronounced, the patient has bleeding, thrombosis, increased size of the spleen and liver.
– Third. Usually begins 15-20 years after the onset of the disease. At this stage, the number of erythrocytes, leukocytes and platelets in the peripheral blood does not increase, but rather decreases, the liver and spleen significantly increase in size, and serious complications develop.
Principles of diagnosing erythremia
Quite often in the early stages, erythremia is asymptomatic. Sometimes it is diagnosed quite accidentally, after a general blood test, which the patient takes for a completely different reason. In this case, the main signs of the disease are
- too high hemoglobin content in the blood (180-220 g / l)
- change in hematocrit, i.e., the ratio of blood formations to plasma (65-80%).
- increase in the number of red blood cells up to 8 million or more in a cubic millimeter of blood (the norm for adults is 4-6 million).
- increase in the number of platelets and leukocytes, decrease in the erythrocyte sedimentation rate (ESR).
Functional diagnostics, such as ultrasound of internal organs, often reveals an increase in the size of the liver and spleen. And additional laboratory tests, which are prescribed when erythremia is suspected, reveal an increase in uric acid concentration, a change in the leukocyte formula, a decrease in erythropoietin – a hormone that regulates the process of red blood cell formation, as well as a mutation in the tyrosine kinase gene JAK2.
Treatment with bloodletting
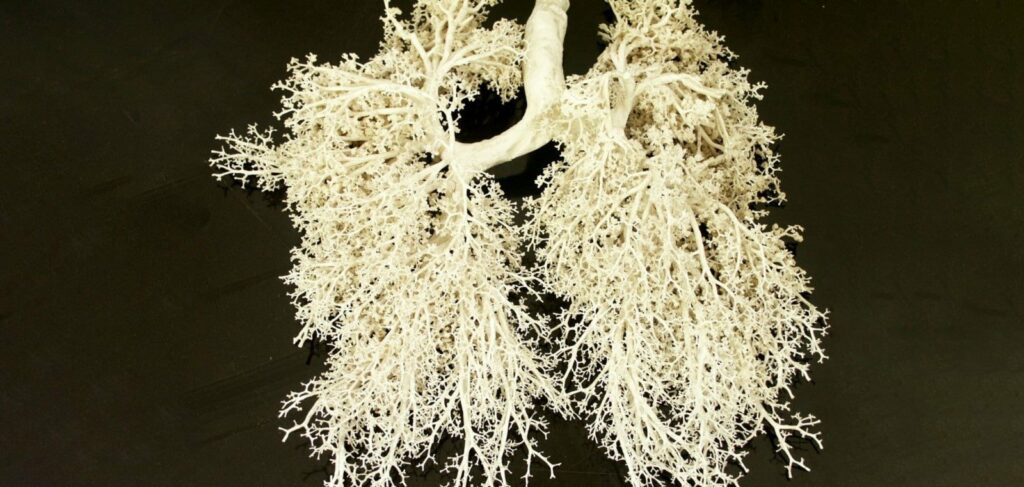
Erythremia is a chronic incurable disease and is fraught with serious and life-threatening complications. First of all, these include thrombotic events, such as embolisms of arterial and venous vessels of the brain, lungs, spleen, and lower extremities. Paradoxically, erythremia sufferers are prone to bleeding, especially with peptic ulcer disease of the stomach and duodenum. They also often develop gallstone disease and liver cirrhosis, increase the risk of nephrosclerosis and kidney stones.
To avoid such severe consequences, it is very important to timely diagnose and properly treat erythremia. The main task of therapy is to normalize the amount of blood. For this purpose, one of the most ancient medical techniques is used – bloodletting, or, using modern terminology, phlebotomy.
It is usually prescribed when the hematocrit is above 55%. At one time, approximately 300-500 ml of blood is removed from the body, repeating the procedure every 2-4 days until the hematocrit drops to 45% for men or 42% for women, and the hemoglobin level does not fall to 140-150 g / l. Notably, bloodletting not only reduces the risk of blood clots, eliminates skin redness and itching, but also improves cognitive function in patients with erythremia.
If phlebotomy does not help or the patient has contraindications to it, such as thrombocytosis, it is replaced by chemotherapy (cytoreductive therapy), which also helps to reduce the red blood cell mass.
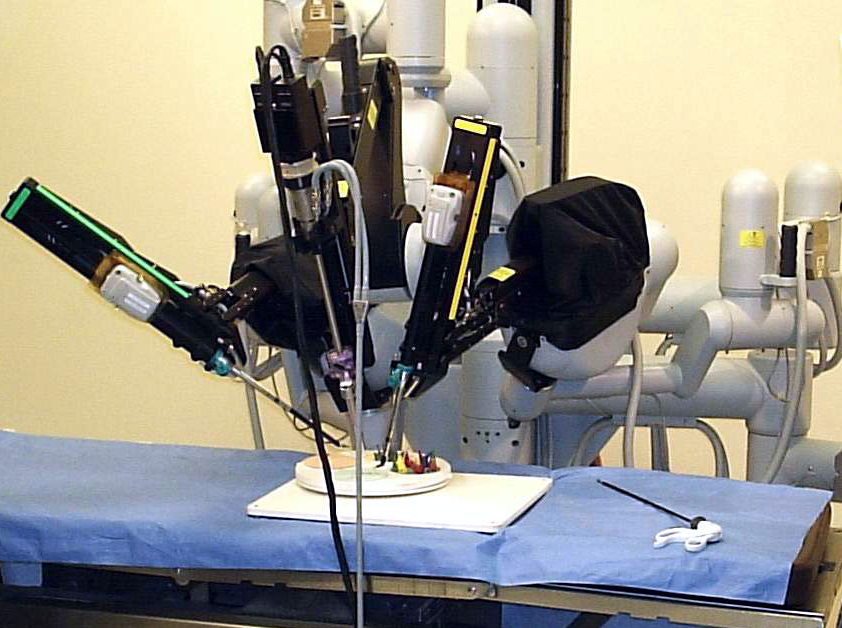
Bloodletting can also be replaced by erythrocytapheresis, or extracorporeal hemocorrection. The best known of its varieties is plasmapheresis. In general, modern hematology has about three dozen methods of extracorporeal hemocorrection.
The treatment regimen for erythremia often includes interferon injections, antihistamines, corticosteroid hormones. To eliminate erythromelalgia and prevent thrombotic complications, low doses of acetylsalicylic acid (75-81 mg per day) or other drugs that reduce platelet aggregation are prescribed.
Today in the West there are ongoing studies of the use of selective inhibitors of tyrosine kinase JAK2, which may help to completely cure or at least block the progression of erythremia. However, such drugs are only in the early stages of clinical trials. And while this disease is considered incurable, it is important to see a doctor at the first sign of it to at least slow down the development of dangerous complications.