We’ll explore the most common causes of post-meal malaise and provide expert tips on managing your symptoms. We will also discuss in detail a possible cause called Dumping Syndrome.
Possible Causes of Weakness and Nausea After Eating
Several factors can contribute to feeling weak and nauseous after meals:
- Low blood sugar (hypoglycemia): If your body produces too much insulin after eating, your blood sugar levels may drop rapidly, causing symptoms like weakness, dizziness, and nausea.
- Food intolerances or allergies: Consuming foods that your body can’t properly digest or that trigger an immune response can lead to nausea, bloating, and fatigue.
- Gastrointestinal disorders: Conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease can cause a range of digestive symptoms, including post-meal nausea and weakness.
- Gastroesophageal reflux disease (GERD): When stomach acid flows back into the esophagus, it can cause heartburn, nausea, and a feeling of fullness or bloating.
- Eating too quickly or overeating: Consuming large meals or eating too fast can lead to indigestion, bloating, and nausea.
When to See a Doctor
While occasional post-meal discomfort is usually not a cause for concern, persistent or severe symptoms may indicate an underlying health issue. Consult your healthcare provider if you experience:
- Frequent episodes of weakness or nausea after eating
- Symptoms that interfere with daily activities
- Unintentional weight loss
- Blood in your stool
- Severe abdominal pain
Your doctor can perform tests to identify the root cause of your symptoms and recommend appropriate treatment.
Managing Symptoms: Diet and Lifestyle Changes
Making simple adjustments to your eating habits can help alleviate post-meal weakness and nausea:
- Eat smaller, more frequent meals: Instead of three large meals, try eating five or six smaller meals throughout the day to avoid overloading your digestive system.
- Chew your food thoroughly: Taking the time to chew your food properly can aid digestion and prevent symptoms like bloating and nausea.
- Identify and avoid trigger foods: Keep a food diary to help pinpoint any specific foods or ingredients that seem to worsen your symptoms, such as dairy, gluten, or high-fat foods.
- Stay hydrated: Drink plenty of water between meals to support healthy digestion and prevent dehydration, which can contribute to weakness and dizziness.
- Manage stress: Stress can exacerbate digestive issues, so practice relaxation techniques like deep breathing, meditation, or yoga to promote overall well-being.
The Role of Probiotics and Digestive Enzymes
In some cases, incorporating probiotics or digestive enzymes into your routine may help alleviate symptoms:
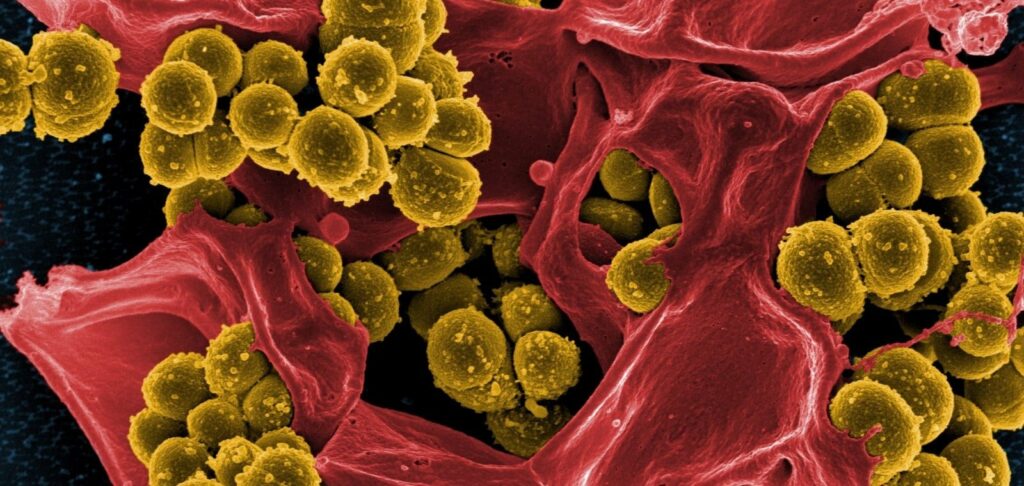
- Probiotics: These beneficial bacteria can help restore balance to your gut microbiome, which plays a crucial role in digestion and nutrient absorption. Probiotic-rich foods include yogurt, kefir, sauerkraut, and kimchi, or you can take a probiotic supplement.
- Digestive enzymes: If your body struggles to break down certain foods, digestive enzyme supplements may help improve digestion and reduce symptoms like bloating and nausea. However, always consult your doctor before starting any new supplement regimen.
What else might it be, Dumping Syndrome?
As you see, there are many reasons why a person might feel nauseous after a meal. If you experience consistent gastrointestinal distress and post-meal weakness that doesn’t improve with diet changes, dumping syndrome may be the culprit
What is Dumping Syndrome?
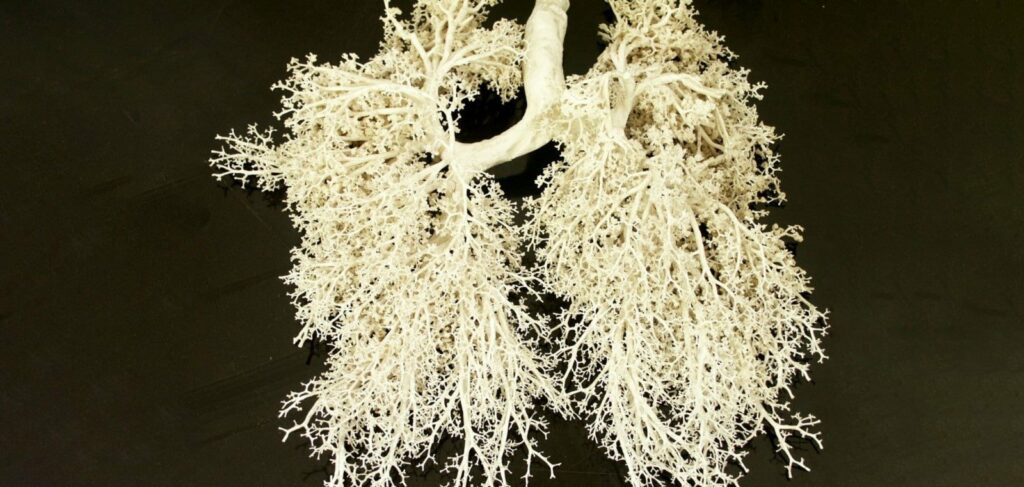
In healthy people, food moves from the stomach to the intestines over the course of several hours. However, with dumping syndrome (from the English word “dumping”), insufficiently digested food is transported (or “dumped”) too quickly from the stomach into the first section of the small intestine – the duodenum.
The overly concentrated chyme (semi-liquid contents of the stomach) causes chemical, physical and osmotic irritation of the duodenal mucosa, which in turn leads to a sharp increase in blood flow in the small intestine. This process is accompanied by decreased blood supply to the brain, lower and upper extremities, as well as hypovolemia, i.e. a decrease in the total volume of circulating blood.
Symptoms of Early Dumping Syndrome
Symptoms of early dumping syndrome include:
- Attacks of general weakness after eating
- Feeling of bloating and distention in the epigastric region
- Dizziness
- Tachycardia
- Shortness of breath
- Sweating
- Tinnitus
- Trembling of the extremities
- Impaired vision
Sometimes these symptoms reach such intensity that a person is simply forced to lie down so as not to fall and lose consciousness. Rapid expansion of the small intestine often causes painful spasms, nausea or even vomiting, as well as osmotic diarrhea.
Risk Factors for Early Dumping Syndrome
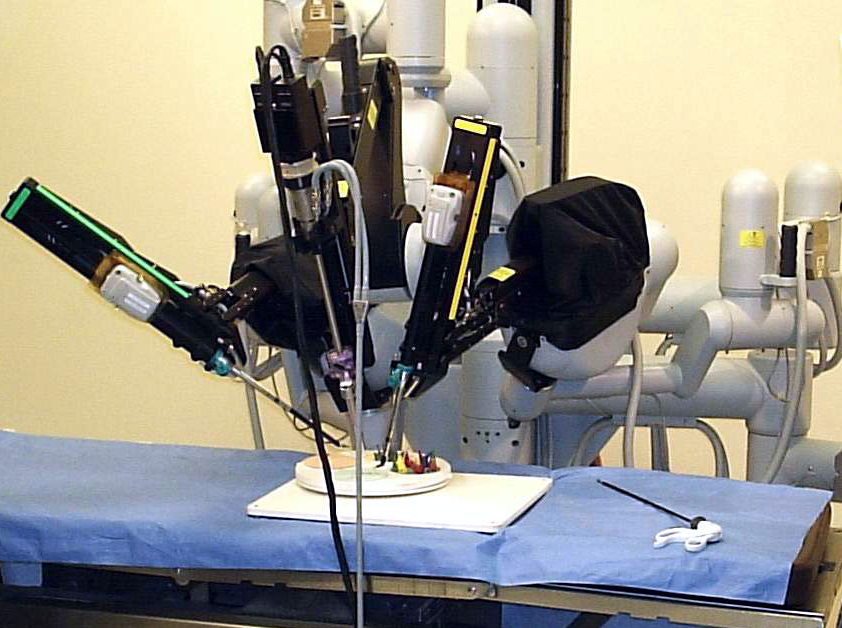
Early dumping syndrome most often occurs as a complication after surgical interventions, such as:
- Gastric resection
- Esophagectomy (removal of part of the esophagus)
- Gastric bypass surgery
It is observed in approximately 15-30% of such patients, and often manifests not immediately, but several years after the operation.
Dumping syndrome can also be associated with anatomical features of the pyloric sphincter between the stomach and duodenum, as well as certain diseases that disrupt its normal function. It is also likely with a condition such as functional dyspepsia, when due to increased contractility of the stomach, its contents enter the duodenum too quickly.
Impact on Nutrient Absorption
Dumping syndrome can affect the absorption of various nutrients. In particular, it can cause a deficiency of:
- Vitamin B12
- Folic acid
- Iron (leading to anemia)
- Calcium (leading to osteoporosis)
Therefore, people suffering from dumping syndrome are often prescribed vitamin and mineral complexes.
Late Dumping Syndrome
Late dumping syndrome has a somewhat different nature. It is also associated with accelerated evacuation of stomach contents, but its trigger mechanism is that in response to the entry of a large amount of food, especially carbohydrates, into the intestine, the pancreas begins to very intensively produce insulin – a hormone that helps the body absorb sugars released from food.
Elevated insulin levels lead to a sharp drop in blood sugar levels within 2-3 hours after eating, causing a condition known as postprandial hypoglycemia. It is usually accompanied by the same symptoms as early dumping syndrome: weakness, dizziness, tachycardia, excessive sweating. A characteristic feature of this condition is an excruciating feeling of hunger.
Late dumping syndrome is usually associated with diabetes mellitus and some other hormonal disorders, as well as taking certain medications that stimulate pancreatic function. And if the patient also has functional dyspepsia, they may experience both early and late symptoms of the disease simultaneously.
Diagnosing Dumping Syndrome
To diagnose dumping syndrome, the doctor must first collect a complete medical and family history (anatomical defects of the pyloric sphincter are often hereditary), and also conduct a number of tests:
- Early form can be detected by a special dumping test – measuring blood pressure and heart rate before and after eating.
- If it gives a positive result, the patient may be prescribed an X-ray examination of the stomach with barium contrast or scintigraphy to confirm the diagnosis.
- Late dumping syndrome is detected using a glucose tolerance test in addition to other methods.
Managing Dumping Syndrome Symptoms
In most cases, the manifestations of dumping syndrome can be eliminated by changing diet and lifestyle. The main rules are:
- Do not overeat or eat until you are full.
- Instead of three meals, it is better to eat five or six times a day in small portions.
- Do not drink water with meals, as too much volume and weight of stomach contents will put strong pressure on the pyloric sphincter, accelerating the transition of chyme into the duodenum.
By following these guidelines and working with your doctor, the unpleasant symptoms of dumping syndrome can be effectively managed in most patients.
Frequently Asked Questions:
What causes sudden weakness after eating?
Is feeling nauseous after eating a sign of diabetes?
How can I prevent feeling dizzy after meals?
In addition to the strategies mentioned, it’s important to understand the potential causes of post-meal dizziness. This condition, sometimes called postprandial hypotension, can occur when blood flow is diverted to the digestive system after eating, temporarily reducing blood supply to the brain. To further prevent this:
- Consider incorporating lean proteins into your meals, as they can help stabilize blood sugar levels.
- Limit alcohol consumption, especially during meals, as it can exacerbate dizziness.
- If you’re on medication, consult your doctor about potential timing adjustments to avoid interactions with meals.
- Engage in light physical activity, such as a short walk, after eating to promote blood circulation.
- Monitor your salt intake, as both too much and too little sodium can affect blood pressure and contribute to dizziness.
- If symptoms persist, keep a food diary to identify potential trigger foods or meals.
What foods help reduce nausea after eating?
Expanding on the foods mentioned, it’s crucial to understand why these options can be beneficial and how to incorporate them effectively:
- Ginger can be consumed in various forms, including tea, candied ginger, or ginger supplements. Its active compounds, like gingerols, have anti-inflammatory properties that can help alleviate nausea.
- Peppermint, whether in tea or candy form, can help relax stomach muscles and reduce bloating.
- The BRATT diet (Bananas, Rice, Applesauce, Tea, Toast) is often recommended for nausea as these foods are easily digestible and can help firm up stools.
- Cold foods like popsicles or smoothies can be soothing and help with hydration.
- Vitamin B6-rich foods, such as nuts and seeds, may help reduce nausea for some individuals.
- Small sips of carbonated water or flat ginger ale can help settle the stomach.
Remember to eat slowly and in small portions when feeling nauseous.
Can anxiety cause weakness and nausea after meals?
What is Dumping Syndrome and how is it treated?
Should I see a doctor if I always feel sick after eating?
When dealing with persistent post-meal sickness, several types of healthcare professionals and alternative medicine specialists might be helpful:
- Primary Care Physician: This should be your first point of contact. They can perform initial assessments and refer you to specialists if needed.
- Gastroenterologist: A specialist in digestive system disorders, they can diagnose and treat conditions like GERD, IBS, or food intolerances.
- Allergist/Immunologist: If food allergies are suspected, this specialist can conduct tests and provide treatment options.
- Endocrinologist: For issues related to hormonal imbalances that might affect digestion.
- Registered Dietitian: Can help identify problem foods and create a suitable meal plan.
- Nutritionist: Offers guidance on overall nutrition and how it affects your health.
Alternative medicine specialists:
Naturopathic Doctor: Focuses on natural remedies and whole-body wellness.
- Acupuncturist: May help with nausea and digestive issues through traditional Chinese medicine techniques.
- Herbalist: Can suggest natural herbs and supplements to aid digestion.
- Functional Medicine Practitioner: Looks at the root causes of symptoms and takes a holistic approach to treatment.
- Ayurvedic Practitioner: Offers treatments based on ancient Indian healing practices.
- Chiropractor: Some specialize in digestive issues and may offer spinal adjustments to improve nerve function related to digestion.
It’s important to note that while alternative medicine can be beneficial, it should not replace conventional medical care.
Always inform your primary care physician about any alternative treatments you’re considering. They can help ensure these treatments don’t interfere with other medical care you’re receiving and can potentially integrate different approaches for the best outcome.