Trimethylaminuria, also known as fish odor syndrome or fish malodor syndrome, is a rare metabolic disorder characterized by a strong, unpleasant body odor reminiscent of rotting fish.
A person with this condition may emit a strong, unpleasant fishy odor from their body fluids, including breath, urine, and sweat.

The smell is often so potent that others may find it difficult to remain in the same room as the affected person, who is usually unaware of their own odor.
This condition can significantly impact quality of life, causing social and psychological distress.
What are the causes, symptoms, diagnosis and management of trimethylaminuria?

Understanding the Causes of Fishy Odor Syndrome
Inherited defect in the FMO3 gene
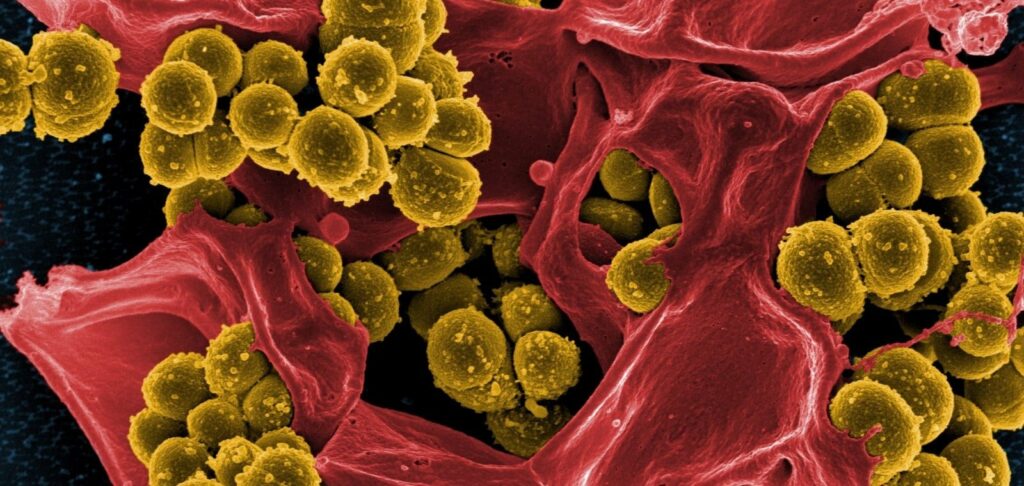
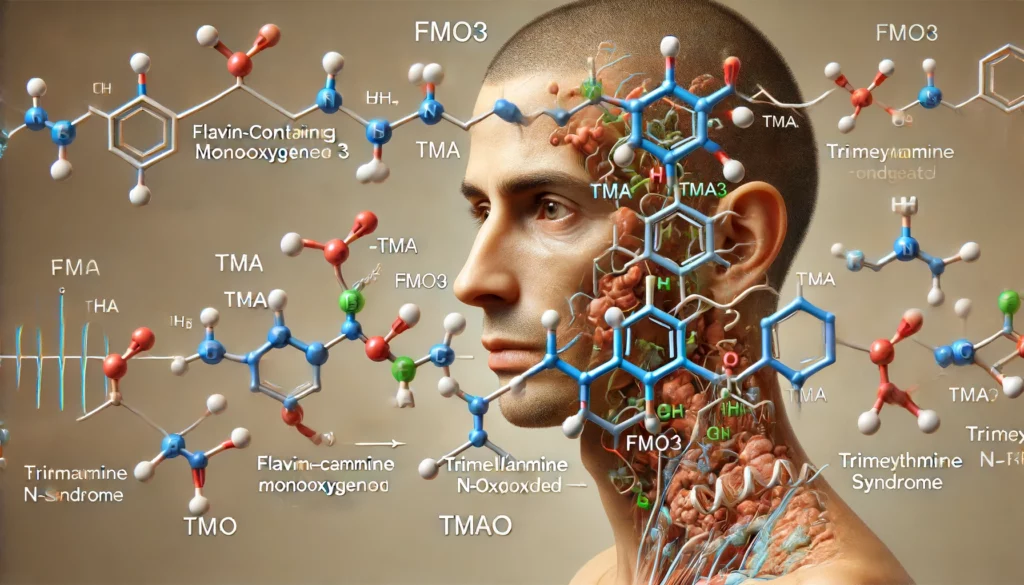
The primary cause of fish odor syndrome is an inherited defect in the FMO3 gene, which codes for the enzyme flavin-containing monooxygenase 3 (FMO3).
This enzyme is responsible for converting odorous trimethylamine, produced by gut bacteria from dietary sources like choline and carnitine, into non-odorous trimethylamine N-oxide.
When FMO3 is deficient or nonfunctional, trimethylamine accumulates in the body and is excreted in sweat, breath, urine and other bodily secretions, resulting in the characteristic fishy smell.

Acquired trimethylaminuria: Medications, vitamin deficiencies, and other factors
In some cases, trimethylaminuria can be acquired due to certain medications (like antidepressants and chemotherapy drugs), vitamin B2 deficiency, liver or kidney disease, and gut dysbiosis.
Dietary factors, such as high intake of marine fish, eggs, offal and legumes, may also exacerbate symptoms by increasing trimethylamine precursor load.
Recognizing the Symptoms of Trimethylaminuria
The hallmark symptom of trimethylaminuria is a strong body odor resembling rotting fish, which can be constant or episodic.
Other signs and symptoms may include:
- Foul-smelling breath, sweat and urine
- Unpleasant taste in the mouth
- Gastrointestinal issues like nausea, vomiting and abdominal pain
- Social isolation, low self-esteem and depression due to embarrassment and stigma
Interestingly, affected individuals often cannot detect their own odor, relying on family and friends to alert them.
Symptoms may worsen during puberty, menstruation, stress, exercise, and after consuming trigger foods.
Infants with trimethylaminuria may exhibit a “sweaty feet” smell and failure to thrive.
Diagnosing Trimethylaminuria: Tests and Challenges
Prompt diagnosis is crucial for initiating appropriate management and support. However, trimethylaminuria is frequently misdiagnosed or underdiagnosed due to lack of awareness among healthcare providers.
The gold standard diagnostic test involves a urine trimethylamine/trimethylamine N-oxide ratio, which is elevated in affected individuals.
This specialized assay is currently available only at select biochemical genetics laboratories like the Research Centre for Medical Genetics in Moscow.
Genetic testing for FMO3 mutations can provide a definitive diagnosis in suspected cases.
Effective Management Strategies for Trimethylaminuria
While there is no cure for primary trimethylaminuria, dietary modifications and lifestyle changes can significantly reduce fishy odor and improve symptoms.
The mainstay of management includes:
- Low-choline, low-trimethylamine diet: Avoiding or limiting high-choline foods like eggs, liver, beans, peanuts, soy, seafood, and cruciferous vegetables. Working with a knowledgeable dietitian to ensure nutritional adequacy is recommended.
- Supplementation: Taking activated charcoal or copper chlorophyllin supplements with meals may help neutralize trimethylamine in the gut. Riboflavin (vitamin B2) supplements can enhance residual FMO3 activity in some patients.
- Odor-reducing strategies: Using pH-balanced soaps and antiperspirants, washing clothes frequently, and maintaining good oral hygiene. Avoiding stress, heat and humidity when possible.
- Gut health optimization: Promoting a balanced gut microbiome through probiotic foods and supplements. Addressing any underlying gastrointestinal issues.
- Medications: In severe cases, short-term use of antibiotics like metronidazole to suppress trimethylamine-producing bacteria, or sequestering agents like cholestyramine, may be considered under medical supervision.
Coping with Trimethylaminuria: Support, Resources, and Advocacy
Coping with the physical, emotional and social challenges of trimethylaminuria can be overwhelming.
Online support groups and resources for patients and families
Fortunately, there are resources and support networks available for affected individuals and their families:
- Online support groups like the UK-based TMAU Support and the US-based National Organization for Rare Diseases provide information, advice and community forums.
- Use telemedicine and online resources like the European Registry and Network for Intoxication Type Metabolic Diseases and MetabERN for expert advice and information.
- Inspirational advocates like British singer-songwriter Cassie Graves, who has trimethylaminuria herself, are working to raise awareness, combat stigma and advocate for better diagnosis and management of this condition.
Specialized care and support in Russia
- Russian Association of Rare Diseases: Information, support, and advocacy for rare disease patients.
- Medical Genetic Scientific Center in Moscow: Specialized diagnostic testing and management for inherited metabolic disorders.
- The Children’s Clinical Hospital of the “Pirogov Russian National Research Medical University” : Comprehensive care for children with rare metabolic disorders.
- Online patient communities like the Russian Patients Association : Forums and resources for rare disease patients.
Specialized care and support in Ukraine
- Consult specialists at the Institute of Molecular Biology and Genetics Institute or
- The Center for Rare Diseases at the Okhmatdyt Hospital in Kyiv for diagnosis and management guidance.
- Connect with the Rare Disease of Ukraine alliance and the Patients of Ukraine organization for support and advocacy.
Empowering Patients to Live Well with Trimethylaminuria
By empowering patients with knowledge, strategies and support, living well with trimethylaminuria is possible.
If you suspect that you or a loved one may have symptoms consistent with this condition, seek evaluation from a healthcare provider specializing in metabolic disorders.
With prompt diagnosis, personalized management and a strong support system, the fishy odor of trimethylaminuria need not define one’s identity or limit one’s potential.