The mysteries of the sphincter of Oddi
Almost 40% of patients after gallbladder removal (cholecystectomy) still have various disorders of the digestive organs. They are called “postcholecystectomy syndrome” (PCES). The most common symptoms are upper abdominal and right subcostal pain, as well as dyspeptic symptoms such as nausea, bloating, constipation or unstable stools. Some patients may experience recurrent hepatic colic and jaundice.
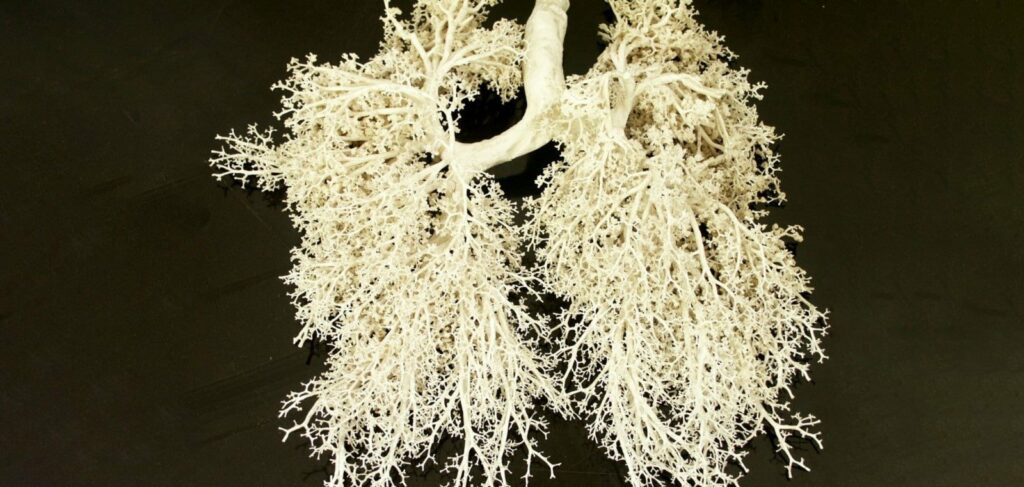
In most cases, these symptoms are related to the fact that the sphincter of Oddi is not functioning properly. This is a special muscle formation, which is a “case” that surrounds the bile and pancreatic ducts at the point where they pass through the duodenal wall. The sphincter of Oddi regulates the timing and frequency of the flow of bile and pancreatic juices into the duodenum, prevents the contents of the small intestine from entering the ducts and ensures the accumulation of bile in the gallbladder. Removal of the gallbladder leads to a change in the tone of the sphincter of Oddi, its spasm. As a result, bile enters the intestine irregularly, digestion and absorption of fats is disturbed, bactericidality of duodenal contents is reduced. This, in turn, entails the appearance of symptoms of dysbacteriosis and chronic inflammatory lesions of the intestine.
In PCES against the background of spasm of sphincter of Oddi and stagnation of bile significantly increases the risk of stone formation in the output ducts of the liver. This is largely due to the fact that after gallbladder removal most patients do not change their food habits, and their diet is still dominated by products that promote stone formation and accumulation of fat in liver cells. Therefore, rapid progression of fatty hepatosis is often observed in PCES.
You have to start with a diet
Treatment of patients with PCES should begin with the transition to dietary nutrition. It is obligatory to follow the diet “table № 5” with low fat content and the exclusion of fried, spicy dishes and acidic foods. It is necessary to limit the use of animal fats as much as possible and increase the proportion of vegetable fats, the advantage of which is the ability to stimulate metabolism in liver cells and reduce the lithogenicity (ability to stone formation) of bile. The addition of dietary fiber to the diet is very useful. Today, pharmacists can offer pumpkin seed meal, several types of pectin in plant fiber and combinations of fiber with elamine, stevia, milk thistle to patients with PCOS.
Prevention of recurrent stone formation
To normalize the biochemical composition of bile, patients with PCES require long-term administration of medications that reduce the concentration of cholesterol and bile acids. Such drugs include ursodeoxycholic acid and chenodeoxycholic acid. After gallbladder removal, the duration of treatment with bile acid preparations should be at least 2-6 months.
Significantly reduce the threat of recurrent formation of stones in the bile ducts, slow the progression of fatty hepatosis allows you to take supplements with lecithin and omega-3 polyunsaturated fatty acids.
Hepatoprotectors play an important role in maintaining good health of patients with removed gallbladder. Products with extracts of milk thistle, melon, rhizomes of Javan turmeric, celandine, turmeric, artichoke are indicated. These preparations not only protect liver cells, but also have choleretic and antispasmodic action.
Pain management
The basis of treatment of PCES and elimination of pain in this condition is the use of drugs that normalize the tone of the sphincter of Oddi, – antispasmodics. It is desirable to recommend buyers myotropic drugs with direct action on the gastrointestinal tract (mebeverine, Drotaverine) or selective blockers of smooth muscle calcium channels (pinaveria bromide). Less effective in sphincter of Oddi dysfunction are non-selective antispasmodics (krasavka preparations, platifylline, benciclone, hyoscine butyl bromide) and selective M1-choline blockers (pirenzepine). In severe pain, short-term administration of NSAIDs is allowed.
Digestive aid
Patients need digestive enzymes to compensate for the enzyme deficiency that develops in PCES. It is recommended to alternate the administration of microgranulated dosage forms of enzymes with preparations containing bile acids.
Since the balance of intestinal microflora is disturbed in all patients after gallbladder removal, the treatment complex includes pre- and probiotics. Among them, the leading place is occupied by probiotics of metabolite type and various combinations of normal intestinal microflora. In case of constipation, the pharmacist may recommend a patient with PCES to take additional lactulose, and in case of diarrheal syndrome – preparations with saccharomyces boulardii.
The predominance of flatulence in the clinical picture of PCES requires the use of medications with “defoamers”. These include various combinations with simethicone and dimethicone. Frequent nausea, belching indicate the development of reflux (reverse peristalsis). In such patients, pharmacists may recommend the prokinetic drug domperidone. If PCES is accompanied by pronounced signs of intoxication, it is advisable to advise the buyer to purchase enterosorbents based on lignin or activated charcoal.
A special place in the treatment of patients with PCES is occupied by mineral waters of weak mineralization – “Naftusya”, “Berezovskaya”, “Morshinskaya”, “Luzhanskaya”, “Polyana Kvasova”. It is allowed to go to water resorts after surgery only after 6-8 months.
In case of frequent recurrence of heartburn and stomach pain after overeating, shoppers may need aluminum-containing buffered antacids or H2-histamine receptor antagonists.
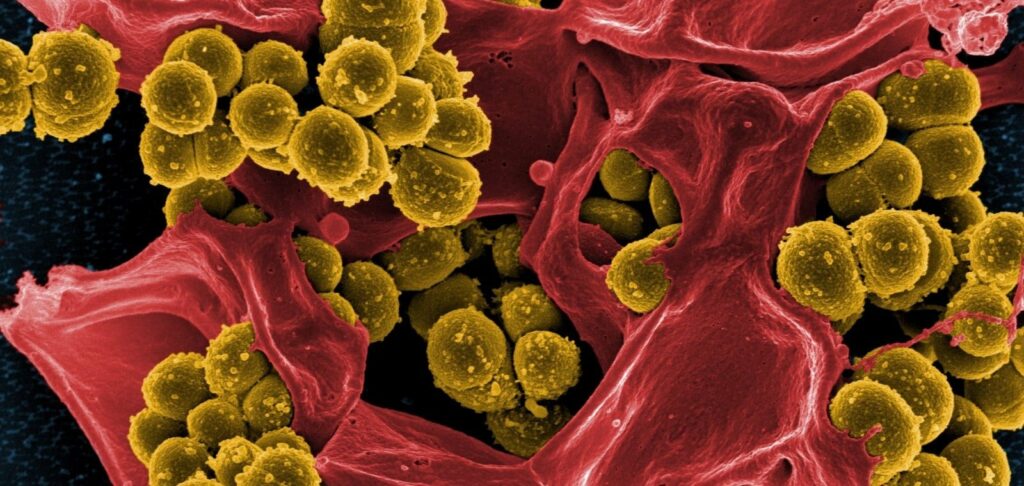
Expressed inflammatory changes in the biliary tract or intestine require a doctor’s examination and prescription of antibacterial drugs. Macrolides, tetracycline preparations, cephalosporins and nitrofurans are indicated.
Diet – Table 5
| You can | You can’t | |
| Bread and flour products | Wheat, yesterday’s pastry (dried) | Fresh, in the form of croutons, pastry products, cakes with cream, chips |
| Meat and poultry | Low-fat varieties (beef, rabbit, chicken, turkey in boiled, baked with pre-boiling); lean ham, doctor’s and diet sausages, sausages | Fatty varieties (pork, goose, duck, game, liver, brains, kidneys) in fried and stewed form; smoked meats, canned foods |
| Fish | Low-fat varieties, boiled, baked with pre-boiling, stuffed, filled with vegetable broth | Fatty species, fried, smoked, salted; canned food, caviar (sturgeon, mullet, Sevryuzha) |
| Eggs | Steamed, baked protein omelet; no more than one yolk per day as part of other meals | In the form of other dishes (hard-boiled, fried) |
| Dairy | Dairy dishes, kefir, yogurt, yogurt, sour curd and dishes from it (pudding, casserole), non-sharp cheese | Whole milk, cream, sour cottage cheese, lazy dumplings, milkshake, fatty homemade sour cream, fatty and salty cheese |
| Fats | Butter, vegetable oil (sunflower, olive oil, corn oil) | Butter, lard, margarine, cooking fats, ghee, overcooked fats |
| Vegetables | In boiled, stewed and baked form, non-acidic sauerkraut | Radishes, turnips, radishes, spinach, sorrel, garlic, raw onions, mushrooms, pickled vegetables |
| Soups | Dairy, vegetable broth with cereals, vermicelli, fruit; vegetarian borscht and shields | On meat and fish broth, mushroom broth; okroshka, green shields |
| Fruit, sweet dishes | Non-acidic berries and fruits, compotes, sours, jellies, mousses, sugar, marshmallows, honey, jam, non-chocolate candies, marmalade | Chocolate, ice cream |
| Sauces and spices | Milk, sour cream, vegetable, fruit and berry gravies, flour for sauce (not toasted), parsley, dill, cinnamon, vanillin | Spicy, on meat and fish broth, mushroom broth; pepper, horseradish, garlic, ketchup, mustard, bite |
| Beverages | Low-strength tea with lemon, vegetable and fruit and berry juices, rosehip decoction | Coffee, cocoa, cold and carbonated drinks |
| Legumes, cereals and pasta products | Buckwheat, rice in the form of porridge, puddings, with the addition of cottage cheese, carrots, other vegetables or fruits, dried fruits; occasionally oatmeal porridge | Millet, barley and pearl porridge, pasta, legumes |
Mode of nutrition: fractional intake five times a day, in a warm form.
Shutterstock/FOTODOM UKRAINE photos used