At the request of our female readers today, we will go into more detail about its causes, symptoms and ways to correct it.
The course is progressive
Genital prolapse (GP) occurs in nearly 30% of women who seek medical attention from a gynecologist. Most often, prolapse of the uterus and vaginal walls develops in those over 50 years of age. In fact, at this age, every second patient has this condition. Among young women, up to 35 years of age, the frequency of GP reaches 10%.
Many specialists consider HP as a type of pelvic floor hernia, in which the normal position of the uterus or vaginal walls is disturbed – they are displaced down to the vaginal entrance and even fall outside it. Such displacement always develops against the background of increased intra-abdominal pressure and failure of the musculo-ligamentous apparatus of the pelvic floor. Starting to form imperceptibly in the reproductive age, GP gradually progresses and over time can lead to a serious deterioration in the quality of life.
Causes and manifestations
The development of HP is determined by many different factors. In addition to age, hereditary weakness of connective tissue (dysplasia); childbirth, especially traumatic; surgical interventions on the pelvic organs; physical work with heavy lifting; chronic inflammatory diseases of the genitourinary system, chronic venous insufficiency; metabolic diseases (obesity, diabetes mellitus, hypothyroidism, etc.) are of great importance.
It has been found that the tone of the pelvic floor muscles and the maintenance of normal position of the internal genitalia are influenced by the level of steroid hormones in the body. In case of imbalance of gonadotropins, corticosteroids and sex hormones with estrogen deficiency GP occurs more often. This is due to the development of atrophy of estrogen-dependent tissues of the lower genitourinary system.
Symptoms of UTIs are diverse and are largely due to the involvement of organs close to the uterus, such as the bladder and rectum, in the pathological process. Women are bothered by periodic pain and heaviness in the lower abdomen, sensations of a foreign body in the vagina, frequent urges and difficulty urinating, menstrual irregularities, secondary infertility. In case of severe prolapse, urinary incontinence, involuntary discharge of intestinal gas and rectal contents are possible.
Therapies
The prognosis and course of genital prolapse largely depend on the stage at which a woman seeks medical help. With minimal prolapse of the internal genital organs, conservative therapy is prescribed, which allows you to slow the progression of pathology. To strengthen the muscles of the pelvic day, back, abdomen, sphincters of the urethra and rectum, it is recommended to systematically perform sets of special physical exercises according to Kegel and Yunosov. Women in menopause are also prescribed hormone replacement therapy.
When indicated, devices that fill the vaginal space are used – tampons, ring-shaped and spherical pessaries. The most convenient and effective are pessaries in the form of a sphere made of synthetic polymer, equipped with a braided nylon band that allows their easy removal. These devices not only support the internal genitalia, but also help to train and strengthen the pelvic floor muscles.
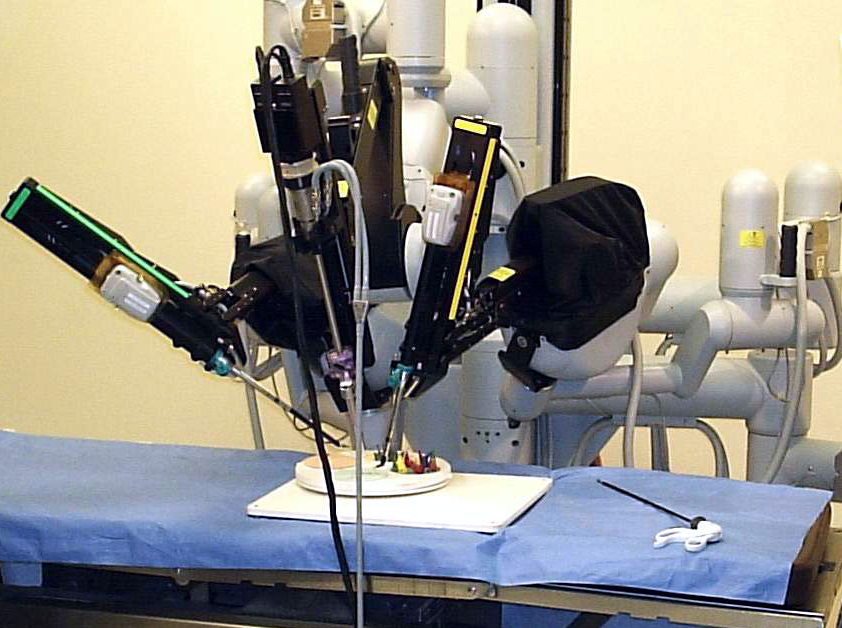
In case of ineffectiveness of physical therapy and conservative therapy, surgical correction of genital prolapse is performed. There are several hundred types and modifications of surgical treatment of uterine and vaginal prolapse. Their choice depends on the degree of GP and the presence of concomitant pathology.