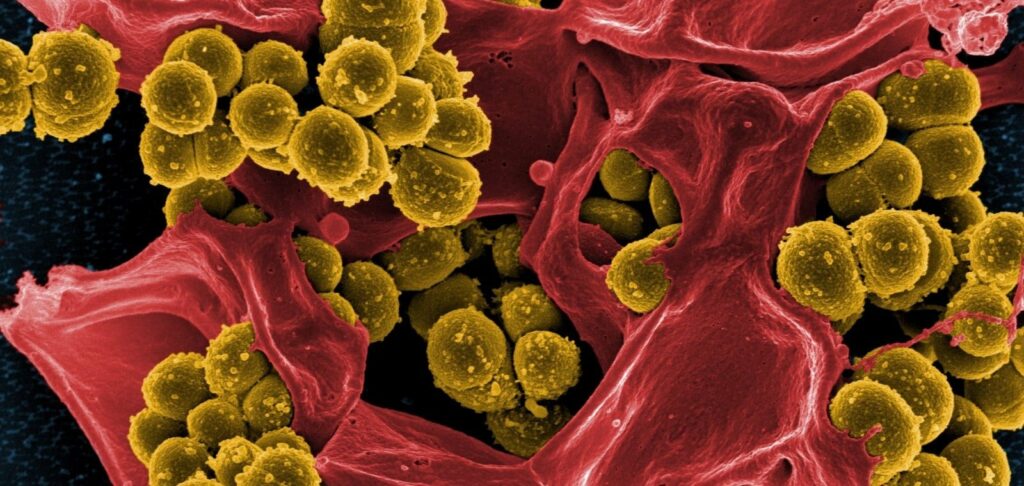
According to the theory of natural selection, the use of any antibiotic eventually leads to the emergence of superbacteria, i.e. microorganisms that, as a result of mutations, become resistant to its effects. Recently, this process has been going too fast, far outpacing the speed of new drug development. Today, more than 700 thousand people a year die because of resistant bacteria in the world, and if the problem is left unattended, the number of deaths will increase to 10 million by 2050. Experts believe that the efforts being made to control superbacteria are insufficient.
Pseudo-allergy to penicillin
Penicillin allergy is believed to be the most common drug intolerance reaction. According to medical statistics, 10% of residents of countries such as the UK or the US have it. However, a number of experts believe that this information may be unreliable, and people who assume they have such an allergy are mistaken. Thus, according to some data, true penicillin allergy, which is accompanied by an IgE-mediated reaction, is very rare and is observed in less than 1% of patients, while anaphylactic reactions occur in only 1-5 cases per 10,000.
Researchers from Harvard Medical School (USA) claim that patients and doctors deal with pseudo-allergy to penicillin in half of cases. It is similar to allergy in symptoms, but has other causes and mechanisms of occurrence, for example, the immune response is not involved, the intolerance reaction begins immediately with the release of the inflammatory mediator histamine. The second half of the adverse reactions occur in patients who did have an IgE-mediated allergy to penicillin, but had already lost sensitivity to the drug years ago. This occurs in about 80% of patients 10 years after the onset of the allergic reaction.
However, even if we are talking about a real allergy, its possible consequences are much less dangerous than refusing to use penicillin drugs. Therefore, experts believe that replacing them with antibiotics of other classes makes sense only when it is an acute, life-threatening allergic reaction, not a trivial rash.
The main problem with widespread pseudoallergy is that it contributes to the growth of resistance of pathogens to antibiotics, that is, the emergence of superbacteria. Penicillin works pointwise and, despite the fact that it was discovered quite a long time ago, retains its activity against many common pathogens. If, due to undesirable reactions, it is replaced by other drugs, then even in minor infections, as a rule, antibiotics of a wide spectrum of activity are used: macrolides, fluoroquinolones, clindamycin, etc. This creates a favorable environment for the emergence of superbacteria. This creates a favorable environment for the emergence and attacks of superbacteria. Thus, according to statistics, patients with poor penicillin tolerance are 30% more likely to be infected with vancomycin-resistant enterococcus, 23% more likely to be infected with Clostridium difficile and 14% more likely to be infected with methicillin-resistant Staphylococcus aureus. The solution to this problem, according to experts, would be to perform samples and tests before each prescription of antibiotics, but for this purpose, affordable test systems must appear on the market, allowing to obtain results in the shortest possible time.
Frustration factor
An unconfirmed penicillin allergy is far from the only factor in the development of drug resistance. Antimicrobial misuse is a huge problem. More than 80% of antibacterial drugs are now prescribed in outpatient medical facilities, but 30% to 60% of prescriptions written are considered suboptimal, and 30% are unnecessary. Most often, doctors unnecessarily prescribe antibiotics for upper respiratory tract infections, such as bronchitis or sinusitis caused by viruses. It is noteworthy that in most cases they do this not because of their own illiteracy, but because of the patients’ persistence. Statistics show that patients who expect to receive a prescription for an antibiotic in advance are three times more likely to leave the doctor’s office with it than those who have no such expectations. Doctors in Western countries fear that if they do not give a patient a prescription, he or she will find the quality of medical care unsatisfactory and will seek help elsewhere.
Recently, this phenomenon, called the “upset factor”, has become a really common phenomenon contributing to the growth of superbacteria. It has gotten to the point where various medical associations have started issuing special guidelines recommending that doctors reduce patient anxiety by changing terminology, for example, calling bronchitis a viral respiratory infection, and increase patient satisfaction by increasing the amount of time spent with the patient, discussing their illnesses in detail, performing a careful examination and ordering additional tests.
Not to stop, but to destroy
Another major problem is poor compliance – patients don’t take their medications as prescribed. People too often stop taking an antibiotic as soon as they feel better. This allows bacteria to develop resistance to a particular drug.A possible solution to the problem, according to experts, would be to keep the price of antimicrobials high enough and change the terms of health insurance. Both economically and psychologically, such a step would increase the value of antibiotics in the eyes of patients. A person who had to pay a decent amount of money for the drug would be more likely to finish the course of treatment.
However, doctors sometimes make mistakes, too. To keep the emergence of drug-resistant strains under control, they must prescribe antibiotics in doses that are high enough to achieve a bactericidal effect. If the microorganisms are killed rather than simply inhibited, mutations that may arise from the antimicrobial agent will not spread.
In and out
In most cases, superbacteria do not pose a serious threat to healthy people and only attack patients whose immune system has been weakened by illness, injury, or surgery. That is why hospital-acquired infections are most often associated with them. The most common vectors of superbacteria from patient to patient are doctors and nurses who do not follow proper hygiene practices, such as hand washing or sterilization procedures.
However, since the mid-1990s, cases of out-of-hospital infections caused by resistant bacteria have also been reported. The first outbreaks were among drug users who injected drugs, but then outbreaks began to occur in any closed system, such as prisons, barracks, student dormitories, sports club locker rooms, or anywhere where people of varying health conditions spent time in confined spaces and practiced poor personal hygiene. When the elderly, immunocompromised, chronically ill patients, and children began to be recorded as having contracted antibiotic-resistant infections, it became clear that the superbacteria were finally out of control.
In order to stop the spread of superbacteria, many developed countries around the world have developed special rules requiring medical personnel to follow infectious disease hospital protocol when a resistant bacterium is detected: use gloves, gowns and masks, wash hands, use disinfectants, and isolate patients to prevent the spread of infection in canteens, bathrooms, elevators and so on.
Controlling the spread of out-of-hospital infections has proved much more difficult, since it is impossible to make people strictly follow sanitary rules without strict supervision of medical personnel. However, timely seeking medical help, obligatory washing and disinfection of even minor wounds, thorough washing and preparation of food, and banal hand washing are exactly what can not only protect against infection, but also prevent the spread of superbacteria in the human population.
People at risk for infection with antibiotic-resistant bacteria include
- Children and the elderly.
- People with weakened immune systems (including patients with HIV, cancer, bronchial asthma, tuberculosis, diabetes, etc.).
- Patients taking broad-spectrum antibiotics.
- Employees and frequent visitors of medical institutions.
- Workers in the field of animal husbandry (cases of infection have been registered in pigs, cattle, poultry).
- People who live in barracks, dormitories, prisons.
- Visitors of tattoo parlors and manicure parlors.
- Beach lovers, visitors to swimming pools and gyms.
- Drug addicts who inject drugs.
Situation with superbacteria infestation in Ukraine
Our country is fully characterized by a worldwide trend of increasing antibiotic resistance. This is largely due to the fact that in a number of pharmacies antimicrobial drugs are sold without prescriptions and even without doctors’ prescription lists.
In other words, people often take such drugs at their own discretion – without appropriate indications, without adhering to the recommended frequency and duration of use. On the other hand, there is a public opinion that antibiotics are harmful to health as such and to the digestive system in particular, which somewhat restrains their uncontrolled use and, consequently, the growth of antibiotic resistance of potentially dangerous microorganisms.
Reliable statistical data on the level of antibiotic resistance of the main pathogens circulating in the population in our territory is rather scarce. This is due to the fact that there is no monitoring and reporting system at the level of medical institutions. In outpatient clinics and hospitals, doctors prescribe antibacterial drugs empirically, i.e. based on their experience, and often urgently. If the patient’s condition does not improve after a few days, an antimicrobial drug of another class is selected.
Determination of sensitivity of pathogens to antibiotics is performed only if it is possible: the patient’s condition is not critical, biomaterial can be taken from him, he is ready to pay for the services of the laboratory, for example, to conduct tests using bacteriostaining or PCR.
To be fair, it should be noted that WHO only in 2015 adopted an action plan to combat antibiotic resistance on a global scale and created a global surveillance system for antimicrobial resistance of superbacteria (GLASS). This system should provide a streamlined approach to collecting, analyzing and disseminating data on antibiotic resistance, which will help create measures to reduce it. Since 2016, Ukraine has been among the countries participating in GLASS. However, the action plan to contain the spread of microbial resistance is still under development, no institution has been designated to coordinate the surveillance network, no reference laboratory has been selected and no funding is available.
In our country, several studies on the problem of antibiotic resistance have recently been conducted, for example, specialists of P.L. Shupyk NMAPO isolated pneumococci resistant to cotrimoxazole, erythromycin and azithromycin from the nasopharynx of healthy children under 5 years of age. These microorganisms may not manifest themselves in the body (asymptomatic carrier), but under certain conditions can become causative agents of meningitis.
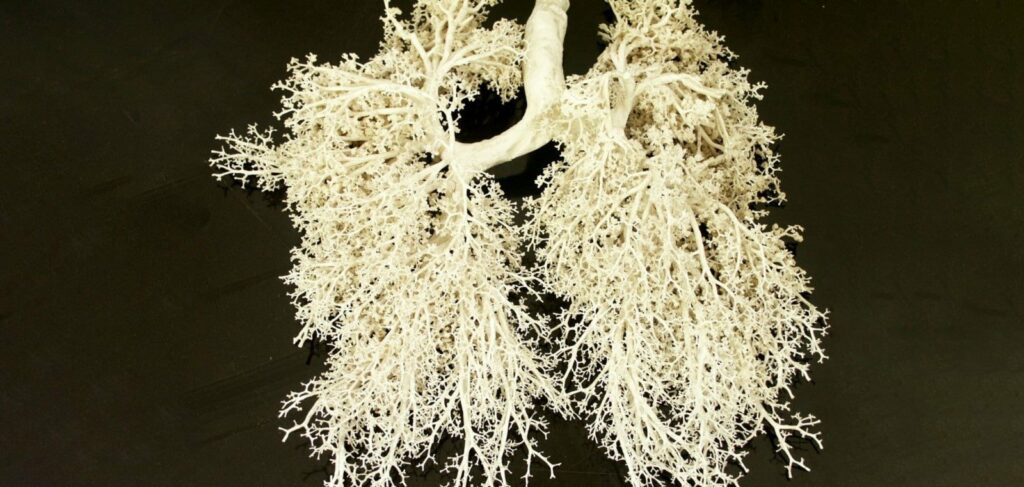
The most significant scientific achievement to date is Ukraine’s participation in 2014-2016 in the international study Survey of Antibiotic Resistance (SOAR), which involves several dozen countries. According to the Journal of Antimicrobial Chemotherapy, the purpose of this stage of work was to determine the sensitivity to antibacterial drugs of pneumococci and Haemophilus bacillus from a number of countries, including 195 strains of S. pneumoniae and 194 strains of H. Influenzae isolated from patients by specialists of the Medical Diagnostic Center of the Medical Academy (Dnipro) and the National Institute of Phthisiology and Pulmonology (Kyiv). It turned out that in general in Ukraine these bacteria, which often cause respiratory diseases, are easier to destroy with antibiotics than similar ones, for example, in the Slovak Republic and the Russian Federation. For example, 97% of S. pneumoniae strains from Ukraine were sensitive to penicillin when administered intravenously, while 83% were sensitive to penicillin when administered orally. Thus, now Ukraine should be more actively involved in the fight against antibiotic resistance – to establish a system of monitoring of detected cases, transfer of regional data to the national and international level, and then implement methods to reduce the resistance of infections to antimicrobial agents, developed by WHO and other organizations. There is also a task for pharmacists: you can explain to pharmacy customers the rules of prescribing and using antibiotics, thus minimizing the number of self-medication cases.