The Urgent Need for Pain Management Reform
The ongoing war in Ukraine has left not only physical scars but also emotional and psychological tolls that cannot be overlooked.
Ukrainian veterans face challenges ranging from physical injuries, like traumatic limb loss, spinal cord damage, and traumatic brain injuries, to mental health concerns such as PTSD, anxiety, and depression.
Effective pain management for these veterans is a complex issue that demands a rethinking of our approach to both physical and emotional pain care—especially considering lessons from the crisis in pain management seen in the United States.

The Complex Nature of Pain Among Veterans
Combat-related injuries among Ukrainian veterans often result in chronic pain conditions that require long-term management.
Chronic pain, in this context, can stem from a combination of physical damage and neurological changes caused by trauma.
Physical injuries can result in ongoing inflammation, nerve damage, and musculoskeletal dysfunctions that all contribute to pain.

Beyond physical injuries, psychological trauma plays a major role in the persistence and perception of pain.
The phenomenon known as “pain catastrophizing,” where negative emotions and anxiety amplify the perception of pain, is particularly common among veterans dealing with PTSD.
This creates a vicious cycle that worsens both pain and mental health conditions.
The lack of integrated mental health and pain management services in Ukraine makes it crucial to consider holistic approaches that address both physical and mental well-being.
The U.S. pain crisis offers valuable insights on what not to do, but also provides pathways for developing more comprehensive solutions.
The U.S. Pain Management Crisis: Key Lessons for Ukraine
The United States is facing an epidemic of chronic pain, compounded by an opioid crisis that has claimed over a million lives.
Estimates indicate that between 21% and 56% of Americans suffer from chronic pain, with a significant portion experiencing pain severe enough to disrupt their daily lives.
Chronic pain often leads to disability, social isolation, and reduced quality of life, creating a burden not only for individuals but also for healthcare systems.
A critical aspect of the U.S. pain crisis is the limited education on pain management in medical schools.
A 2018 systematic review found that most American medical schools dedicate fewer than ten hours to pain management throughout their entire curriculum.
As a result, many doctors rely heavily on pharmaceuticals, particularly opioids, as they lack knowledge of other options.
This has led to over-prescription and addiction issues, and a fear of legal repercussions has led many to avoid prescribing opioids altogether, leaving many pain patients untreated.
These issues underscore the risks of relying solely on pharmaceutical interventions for pain relief.
Opioid medications carry risks of addiction, immune suppression, increased risk of accidents, and even a paradoxical increase in pain over time, known as opioid-induced hyperalgesia.
Other pharmaceutical options, such as gabapentinoids, antidepressants, and NSAIDs, also come with significant risks of side effects and often fail to address the underlying causes of chronic pain, leaving patients with limited and often unsatisfactory options.
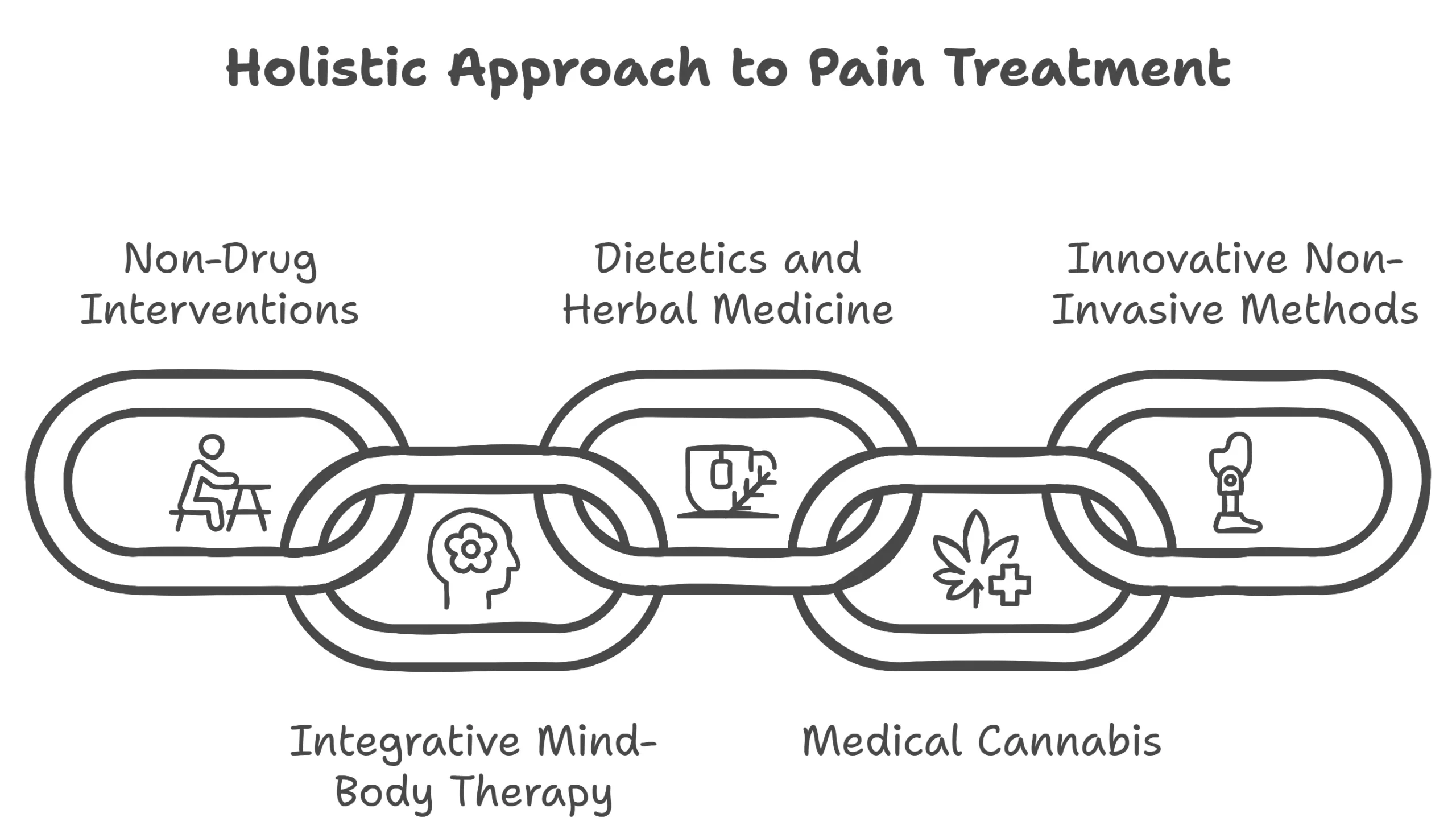
A Holistic Approach to Pain Management for Ukrainian Veterans
The challenges faced in the U.S. should serve as a warning for Ukraine. Ukrainian veterans deserve a comprehensive, compassionate approach to pain care that doesn’t replicate the pitfalls seen elsewhere. Specifically, a reliance solely on pharmaceuticals is unlikely to succeed.
Instead, a diverse range of treatments should be considered, including:
1. Non-Pharmacological Interventions
Treatments like physical therapy, exercise programs, and massage therapy can address musculoskeletal imbalances, which are often the source of chronic pain.
Physical therapy helps in restoring movement and function to parts of the body affected by injury or surgery, while exercises tailored to the individual can help in strengthening muscles and improving flexibility, ultimately reducing pain.
Physical activity, though sometimes daunting for individuals in pain, has been shown to improve pain outcomes and quality of life.
It helps release endorphins, which are natural painkillers produced by the body, and reduces the inflammation often responsible for pain.
It’s essential for healthcare providers to encourage veterans to engage in physical activities that are appropriate for their specific conditions, focusing on gradual progression to avoid exacerbating injuries.
2. Integrative Mind-Body Therapies
Chronic pain is often deeply intertwined with mental health issues, such as PTSD.
Psychotherapy, particularly trauma-informed cognitive behavioral therapy (CBT), can help veterans process their experiences and, in turn, mitigate their physical pain.
Trauma-informed CBT helps patients reframe their relationship with pain, reducing catastrophizing and improving coping mechanisms.
Mind-body therapies such as mindfulness meditation, biofeedback, and neurofeedback can also be highly effective.
Mindfulness meditation has been shown to alter pain perception by changing the brain’s response to pain signals, allowing veterans to experience pain with less emotional reactivity.
Biofeedback helps patients learn to control physiological functions such as muscle tension, which can reduce pain levels.
Neurofeedback, which involves training the brain to function more optimally, can also be beneficial for veterans dealing with chronic pain and PTSD.
3. Nutritional and Herbal Therapies
Chronic pain can often be exacerbated by inflammation, which may be influenced by diet. Diets high in processed foods, sugars, and unhealthy fats are known to increase inflammation, whereas anti-inflammatory diets—rich in fruits, vegetables, omega-3 fatty acids, and lean proteins—can help in managing pain.
Nutritional guidance, possibly provided by nutritionists or integrative physicians, could help veterans manage inflammation and improve their overall health.
Herbal medicine also provides promising alternatives. Turmeric, ginger, and other anti-inflammatory herbs have been shown to reduce pain without the severe side effects seen in pharmaceutical drugs.
4. Medical Cannabis
Medical cannabis offers pain relief for certain conditions such as cancer, epilepsy, chronic pain, and PTSD, particularly for veterans affected by the ongoing war with Russia.
In Ukraine, medical cannabis can only be prescribed when other treatments have failed or are poorly tolerated, making it a secondary but important option for those with persistent symptoms.
The Ministry of Health has approved several forms of cannabis-based medicines that can be manufactured in pharmacies, including oral liquids, capsules, and gels. These medicines are available only through electronic prescriptions from licensed doctors, ensuring that they are used under proper medical supervision.
Medical cannabis not only provides pain relief but also helps reduce anxiety and improve sleep, both of which are crucial for veterans dealing with chronic pain and PTSD.
5. Innovative Non-Invasive Treatments
Technologies such as red/infrared light therapy, pulsed electromagnetic field therapy (PEMF), and hyperbaric oxygen therapy (HBOT) are gaining traction as safe, effective options for pain management.
- Red/Infrared Light Therapy: This therapy works by using specific wavelengths of light to penetrate tissues and reduce inflammation and pain. It has been shown to stimulate the mitochondria, boosting cellular repair and promoting healing, which can be especially beneficial for veterans with musculoskeletal injuries.
- Pulsed Electromagnetic Field Therapy (PEMF): PEMF works by using electromagnetic fields to stimulate the body’s cells, promoting healing and reducing pain. PEMF can be useful for treating joint pain, muscle pain, and other forms of chronic pain by improving blood circulation and enhancing the body’s natural recovery processes.
- Hyperbaric Oxygen Therapy (HBOT): HBOT involves breathing pure oxygen in a pressurized environment, which increases the amount of oxygen in the blood and promotes faster healing. It is effective for reducing inflammation, promoting tissue repair, and can be particularly useful for treating wounds and injuries sustained during combat.
The Importance of Physician Education and Veteran-Centric Care
One of the key lessons from the U.S. crisis is the necessity of proper physician education. Medical professionals need more than a few hours of training in pain management—they need a robust understanding of both pharmacological and non-pharmacological options to truly serve their patients.
This includes understanding when and how to use alternative therapies, and how to create an individualized care plan that addresses not just physical pain but also psychological and social factors.
Physicians treating Ukrainian veterans must be open to alternative therapies and should seek additional education in holistic care.
This may involve attending workshops, taking courses in integrative medicine, or collaborating with specialists in fields such as physical therapy, psychology, and nutrition.
By expanding the tools available to them, physicians can create more personalized, effective pain management plans for veterans, thus avoiding the pitfalls seen in the U.S. system.
The goal should be to treat the whole person, not just the symptoms.

A Holistic and Compassionate Path Forward
The need for action is urgent. Ukrainian veterans are battling visible and hidden wounds. Without comprehensive change, too many will suffer in silence.
But there is hope. By embracing a holistic approach—integrating physical therapies, mental health support, nutrition, and innovative technologies—we can transform pain care in Ukraine.
We can alleviate pain, restore dignity, and improve veterans’ quality of life—but only if we act now.
Now is the time for Ukraine to lead by example.
With determination and empathy, we can help veterans reclaim their lives, reconnect with loved ones, and reintegrate into their communities.