The Rise of Peanut Panic
A Tale of Two Worlds: Peanut Allergies in CIS Countries and the USA
In countries like Russia, Ukraine, Kazakhstan, and the Caucasus region, peanut allergies exist but remain relatively rare.
Parents in these nations occasionally approach pediatricians with worried questions about introducing peanuts to their children’s diets. Doctors typically advise caution, recommending gradual introduction and careful observation for any adverse reactions.
However, the overall threat level is perceived as low, and peanut-related panic is far from the norm.
Interestingly, medical professionals in these countries are aware of the dramatically different situation in the United States. Many find themselves puzzled by the stark contrast: Why are peanut allergies so prevalent in America while remaining relatively uncommon in their own practices?
This disparity has led to a growing curiosity about the factors that might have contributed to such different outcomes.
So, what’s happening in America?
How did the United States, a country known for its advanced healthcare system, inadvertently spark a peanut allergy epidemic?
How did peanuts, once a beloved snack and a staple of childhood nutrition, become Public Enemy Number One in the realm of food allergies?
The Birth of a Health Crisis
To understand this paradox, we need to turn back the clock to the late 1990s. It was during this period that the United States witnessed a curious and alarming development. Media outlets began reporting on children who had suffered severe, sometimes fatal, reactions to peanuts.
These stories, while tragic, were statistically rare. In 1999, researchers at Mount Sinai Hospital estimated the incidence of peanut allergies in children to be a mere 0.6%.
However, the impact of these reports was seismic. The medical community took notice, and suddenly, peanut allergies became a hot topic of discussion among pediatricians.
Parents, understandably concerned about their children’s safety, began to ask questions.
What could be done to prevent these allergies? How could they protect their children from this seemingly random and potentially lethal threat?
The Academy of Pediatricians Takes Action
Responding to this growing public concern, the American Academy of Pediatrics (AAP) decided to take action.
In 2000, they issued a recommendation that would change the course of childhood nutrition in America:
Children under 3 years old, as well as pregnant and lactating mothers, should avoid all peanuts.
This advice seemed logical at the time. After all, if peanuts were causing allergies, wouldn’t avoiding them solve the problem?
The AAP was following in the footsteps of the UK’s health department, which had made a similar recommendation two years earlier.
However, there was a crucial flaw in this approach: The recommendation was based on precaution rather than solid scientific evidence.
The AAP committee admitted that “the ability to determine which infants are high-risk is imperfect.”
In essence, they were casting a wide net, hoping to catch and prevent all potential cases of peanut allergy.
From Recommendation to Dogma
What started as a cautious recommendation quickly transformed into medical dogma.
Pediatricians across the country adopted a simple mnemonic to teach parents: “Remember 1-2-3. Age 1: start milk. Age 2: start eggs. Age 3: start peanut products.”
Many well-meaning doctors and parents, erring on the side of caution, interpreted this guideline in the strictest possible terms. Why take chances with something as serious as a potential food allergy?
This led to a generation of children growing up in households where peanuts were treated like a dangerous substance, to be avoided at all costs.
The ripple effects of this recommendation were far-reaching. Food manufacturers began prominently labeling their products to indicate the presence or absence of nuts.
Schools started implementing peanut bans, creating “nut-free zones” in cafeterias. The humble peanut butter and jelly sandwich, once a lunchbox staple, became a controversial item.
Little did the AAP know that their well-intentioned recommendation, aimed at protecting children, would set the stage for an unprecedented allergy epidemic.
The peanut, once a beloved snack, had become the focal point of a nationwide health panic.
The Unintended Consequences
When Prevention Becomes the Problem
As the new millennium dawned, the American Academy of Pediatrics’ recommendation to avoid peanuts in early childhood was in full effect.
Parents across the nation diligently kept peanut products away from their young children, believing they were safeguarding them against a potentially life-threatening allergy.
However, as time passed, a disturbing trend began to emerge.
By 2004, just four years after the AAP’s recommendation, it became clear that the rate of peanut allergies was not decreasing as hoped. Instead, it was soaring at an alarming rate.
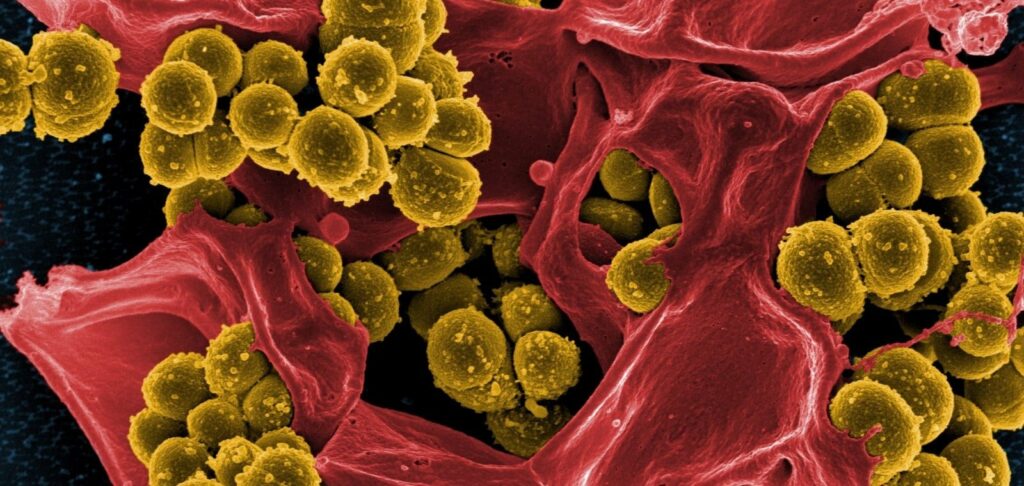
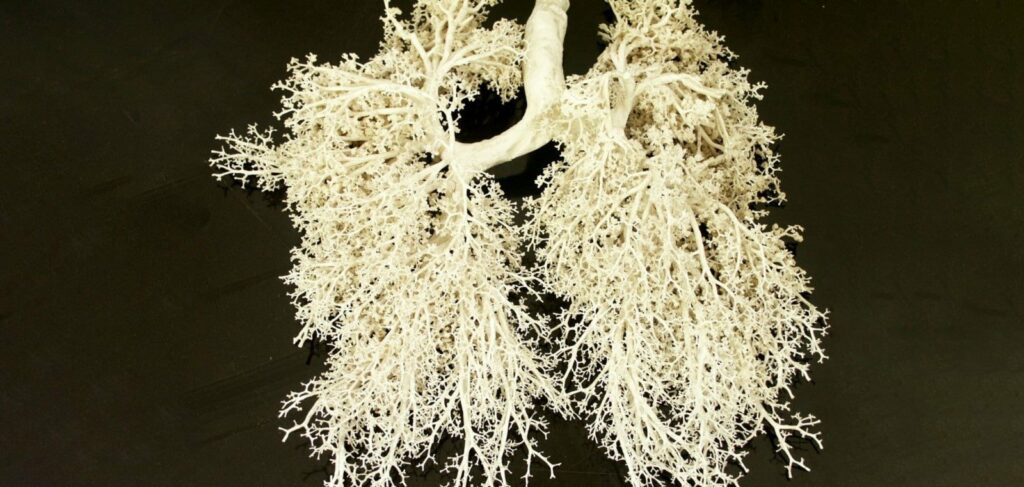
Emergency department visits for peanut anaphylaxis – a life-threatening allergic reaction causing severe swelling of the airways – skyrocketed.
The Numbers Tell a Startling Story
The statistics were staggering. In 2016, the Parkway School District in St. Louis County, Missouri, reported 957 students with documented life-threatening food allergies, most of which were to peanuts.
This represented a 50% increase from just six years prior, and an astonishing 1,000% increase from the previous generation.
Schools across the country responded by enacting increasingly stringent peanut bans. What was once a common lunchbox item became contraband in many educational institutions.
The humble peanut had been transformed from a nutritious snack into a perceived public health threat.
The Rise of the EpiPen
As peanut allergies became more prevalent, so did the need for emergency treatment. Enter the EpiPen, an auto-injector device containing epinephrine, used to treat severe allergic reactions. Sales of EpiPens soared, and pharmaceutical companies took notice.
In a move that would later spark controversy, Mylan Pharmaceuticals dramatically increased the price of EpiPens. And why not, it was needed for these medical emergencies??
The cost in the U.S. rose to $600, compared to just $30 in some other countries. This price hike added financial strain to the already considerable burden faced by families dealing with peanut allergies.
A Self-Fulfilling Prophecy?
As the situation worsened, many public health leaders doubled down on their stance.
They reasoned that if only every parent would comply with the pediatrics association guideline, the country could finally win the war against peanut allergies. This thinking led to even more aggressive avoidance strategies and public awareness campaigns.
However, this approach seemed to be creating a self-fulfilling prophecy. The more that health officials implored parents to follow the recommendation, the worse peanut allergies got.
From 2005 to 2014, the number of children going to the emergency department because of peanut allergies tripled in the U.S.
The Hidden Cost of Avoidance
Beyond the immediate health concerns and financial costs, the peanut avoidance strategy was having other, less visible effects on society. Children with peanut allergies often faced social isolation, unable to participate fully in school activities or birthday parties due to fear of exposure.
Parents of allergic children lived in constant anxiety, always on high alert for potential allergen contact.
Moreover, the focus on peanut avoidance was diverting attention and resources from other important childhood health issues.
The medical community found itself caught in a cycle of reaction and escalation, continually increasing preventive measures as allergy rates continued to climb.
A Paradigm in Need of Shifting
By 2019, a report estimated that 1 in every 18 American children had a peanut allergy. This represented a public health crisis of significant proportions, one that showed no signs of abating despite years of concerted efforts to prevent it.
It was becoming increasingly clear that something was fundamentally wrong with the prevailing approach to peanut allergies.
The strategy of avoidance, conceived with the best of intentions, seemed to be exacerbating the very problem it was meant to solve.
As the crisis deepened, a growing number of researchers began to question the wisdom of the peanut avoidance paradigm.
Was it possible that in trying to protect children from peanut allergies, the medical community had inadvertently created the perfect conditions for those allergies to thrive?
The stage was set for a radical rethinking of the peanut allergy problem.
Challenging the Status Quo and Finding Solutions
A Eureka Moment in Israel
As peanut allergies continued to surge in the United States and United Kingdom, a curious observation was made across the globe.
In 2000, Dr. Gideon Lack, a pediatric allergist and immunologist in London, was giving a lecture on allergies in Israel. He asked the audience of roughly 200 pediatricians, “How many of you are seeing kids with a peanut allergy?”
To his astonishment, only two or three hands were raised. This stood in stark contrast to his experiences in London, where nearly every pediatrician would have raised their hand to the same question.
This discrepancy sparked a eureka moment for Dr. Lack. He recalled that many Israeli infants are regularly fed Bamba, a popular peanut-based snack.
Could there be a connection between early peanut exposure and the low rate of peanut allergies in Israel?
Groundbreaking Research Challenges Conventional Wisdom
Intrigued by this possibility, Dr. Lack quickly assembled a team of researchers in Tel Aviv and Jerusalem to launch a formal study.
The results were striking: Jewish children in Israel had one-tenth the rate of peanut allergies compared to Jewish children in the UK.
This finding suggested that genetic predisposition, long assumed to be a primary factor in peanut allergies, was not the whole story.
In 2008, Lack and his colleagues published their findings in a paper titled “Early Consumption of Peanuts in Infancy Is Associated with a Low Prevalence of Peanut Allergy.”
However, despite the implications of this research, it wasn’t enough to immediately uproot the deeply entrenched groupthink surrounding peanut avoidance.
The LEAP Study: A Paradigm Shift
Undeterred, Dr. Lack continued his research. In 2015, he published the results of a second clinical trial in the New England Journal of Medicine.
This study, known as the Learning Early About Peanut Allergy (LEAP) trial, compared two groups of infants:
- Those exposed to peanut butter at 4-11 months of age
- Those who had no peanut exposure, following the AAP recommendation
The results were nothing short of revolutionary.
Early exposure to peanuts resulted in an 86% reduction in peanut allergies by the time the child reached age 5, compared to children who followed the AAP recommendation of avoidance.
The Medical Community Grapples with New Evidence
The LEAP study sent shockwaves through the medical community.
Dr. Drew White, an allergist at the Scripps Clinic in San Diego, summed up the reaction of many in the field: “After it came out, we immediately thought, ‘How are we going to fix this giant mess?'”
The absolutism of the AAP’s 2000 recommendation had made it difficult to walk back.
Many in the medical community found themselves grappling with a hard truth: their well-intentioned advice may have contributed to the very epidemic they were trying to prevent.
A Lesson in Medical Humility
The peanut allergy epidemic serves as a stark reminder of the dangers of medical dogma.
When modern medicine issues recommendations based on robust scientific studies, it can achieve remarkable results.
However, when doctors rule by opinion and edict without sufficient evidence, the consequences can be dire.
The original AAP recommendation could have been more tentative, acknowledging the uncertainty surrounding peanut allergies.
A simple “We’re not sure” might have prevented years of misguided advice and its unintended consequences.
The Path Forward
In light of the new evidence, health organizations began to revise their guidelines. In 2017, the National Institute of Allergy and Infectious Diseases (NIAID) issued new clinical guidelines recommending early introduction of peanut-containing foods to infants to prevent peanut allergy.
However, changing deeply ingrained behaviors and beliefs takes time. The peanut allergy reputation was built over time. As long as people avoid peanuts, the allergies will continue to develop.