Abandon the “arms race”
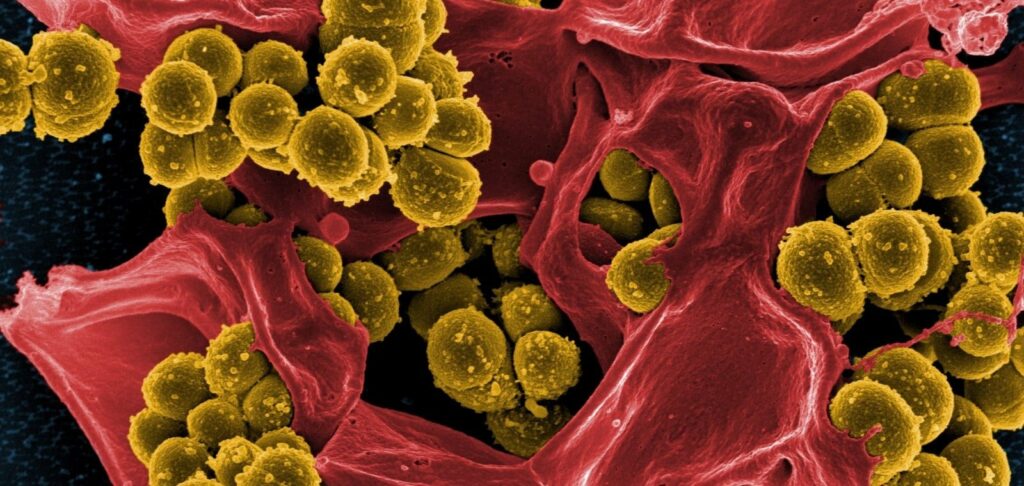
The global pharmaceutical industry has not been able to respond adequately to the growing number of superbacteria and the increased mortality associated with them. We are talking about infections such as Acinetobacter, methicillin-resistant Staphylococcus aureus, Pseudomonas, Salmonella, etc. New antibiotics for the treatment of diseases caused by them are becoming increasingly rare, and even measures to accelerate their introduction into clinical practice cannot dramatically improve the situation.
In this regard, the scientific community is increasingly suggesting that there is no point in indefinitely improving “weapons” against bacteria, as they easily adapt to the action of antibacterial drugs, i.e. find ways to remain invulnerable. Instead of an “arms race”, a number of researchers propose to concentrate on finding and using other, more environmentally friendly mechanisms to protect the human body from dangerous infections that exist primarily in the human body. This idea is based on the fact that, as a biological species, Homo sapiens has interacted for several millennia with a huge world of bacteria, including agents of terrible epidemics, but has survived. In other words, microorganisms become highly virulent and very dangerous to humans under certain unfavorable conditions. If such factors are known and their influence is eliminated, mortality from infectious diseases will be reduced.
The situation with plague, which has killed hundreds of millions of people in Europe, Asia and the Americas over several centuries, is a striking example. Its causative agent Yersinia with fleas is transmitted to humans mainly from rodents (rats, ferrets, gophers, etc.). In the Middle Ages, large-scale epidemics occurred after mass migration of such animal carriers due to sudden cold or famine. But in areas where infected individuals lived permanently, as a rule, there were no terrible epidemics. People there recorded a small form of plague, which was manifested by enlarged lymph nodes, increased body temperature, headache and passed like a cold, within a week. It turns out that the human body has a reliable defense even against plague, you just need to know how to activate it.
Unexpected patterns
The interactions between the human body and pathogenic bacteria are complex and surprising. It would seem that immunity factors always fight infections, and those, in turn, only harm the body. However, these are not axioms at all. Thus, neutrophils (leukocytes) should absorb pathogenic bacteria, break them down inside themselves, and then die off. In the case of Pseudomonas biofilms, things are somewhat different: white blood cells attack these “bacterial cities”, die and… become “building material”. Pseudomonas bacillus uses human immune cells to increase its numbers and develop biofilms. These, by the way, are created by up to 60% of all pathogenic bacteria, so many of them become the cause of chronic diseases and are virtually inaccessible to antibiotics.
There is an opposite example: Salmonella has been found to contain a protein whose task is to block the signals that the intestine sends to the brain demanding that a person stop eating. It turns out that Salmonella “cares” that the infected person receives nutrients and remains alive – this is the key to its survival and reproduction.
Many such unexpected patterns in the interactions between the human body and pathogenic bacteria have already been studied, substances and factors with protective properties have been identified, and they may become an effective alternative to antibiotics in the future.
Promising prospects that will defeat superbacteria
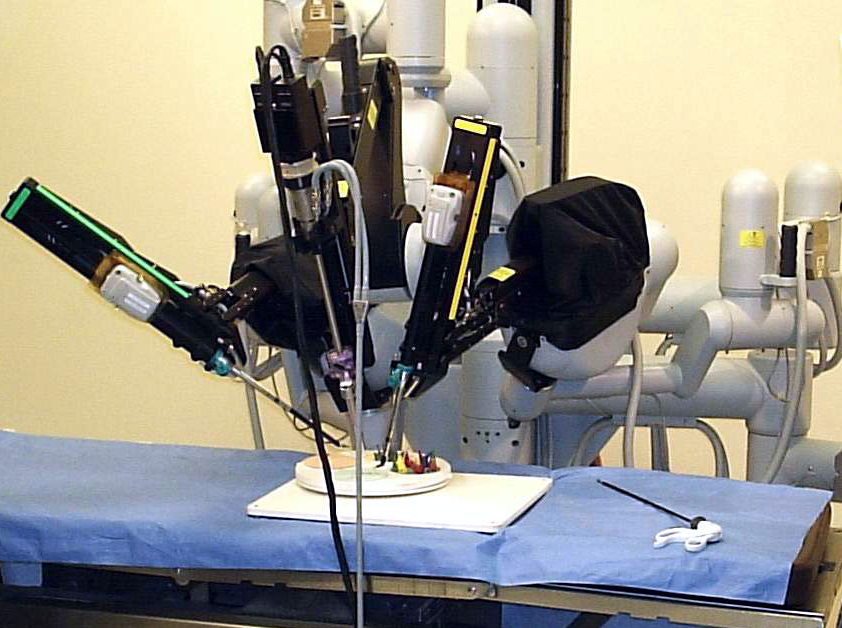
Work is now underway on a number of priority areas and new tools are being developed that will act on the pathogens or the organism affected by them.
– Antibodies. These are highly precise weapons of the immune system against specific pathogens. Antibodies bind to bacteria and inactivate them or their virulence factors and toxins. Antibody-based drugs have already been developed, and about 10 of them are currently undergoing various stages of clinical trials. Last year, the FDA approved one of these drugs, bezlotoxumab, designed to prevent recurrent infections caused by Clostridium difficile bacteria (occurring in 25-30% of cases). Clostridium difficile causes diarrhea, which can be fatal in debilitated patients. Bezlotoxumab is an antibody whose action is aimed at neutralizing the toxins that are produced by C. difficile and provoke the disease. It is noteworthy that the course of treatment is only one injection of the drug.
– Probiotics. Live microorganisms (lacto- and bifidobacteria) that, when properly strained and administered in adequate amounts, enhance the health of the human body by influencing local immunity in the gut. Probiotics help to displace pathogens throughout the body and also synthesize bacteriocins, lysozyme and other antimicrobial substances. In a few years, probiotics effective for diarrhea caused by C. difficile should be available.
– Bacteriophages are natural and artificial. These are viruses directed against certain pathogenic bacteria. The selective action of phages is due to the fact that, thanks to their sensors, they bind to the receptors of bacterial cell walls, penetrate bacterial cells and switch them to reproduction of their own kind. With the help of genetic engineering methods phages are improved, giving them new properties. Thus, it is expected that by 2023 bacteriophages capable of fighting P. aeruginosa will be registered.
– Bacteriolysins. These substances, as their name implies, dissolve bacteria. For pharmaceutical production, substances used by bacteriophages to destroy bacterial cell walls are promising. Lysins are particularly active against Gram-negative pathogens. Two lysine preparations are currently undergoing Phase I clinical trials for the treatment of diseases caused by resistant Staphylococcus aureus.
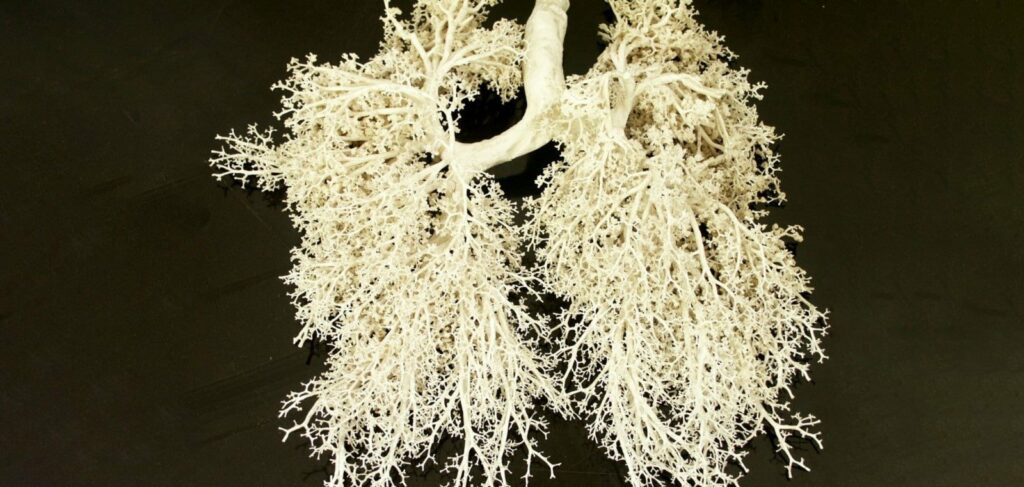
– Enzymes. The functions of both the immune system and pathogens are largely controlled by enzymes. These substances trigger some processes and inhibit others, which can be used in the development of a new class of antibacterial drugs. For example, the enzyme oligoribonuclease inhibits the exchange of chemical signals between individual bacteria. It can be used to stop or prevent the formation of biofilms at the early stages of their formation.
– Immunomodulators. We are not talking about means that increase nonspecific immunity, but about more complex matters. The fact is that the success of antimicrobial therapy depends on a proper immune response. Sometimes it is necessary to enhance it, and for this purpose it is planned to use bacterial lysates, for example, probiotic strains, which are superior to live probiotics in a number of properties. And in the case of septic shock, it may be necessary, on the contrary, to reduce the excessive immune response to reduce tissue damage due to the action of pro-inflammatory cytokines. Such drugs are still under study.
– Vaccines. Work is underway to develop vaccines aimed at new “targets,” such as resistant Staphylococcus aureus, to reduce the need for new antibiotics. Notably, these drugs would be designed to immunize not only children but also adults, including the elderly and debilitated patients. Several such vaccines are already undergoing Phase II and Phase III clinical trials.
– Antimicrobial peptides. There are no such outstanding achievements in this area of research yet, but it is very promising in terms of creating fundamentally new drugs. The essence here is to involve in the fight against infections small protein molecules, which are factors of the innate immunity system of the human body. Antimicrobial peptides have an indirect effect: they protect the skin, GI tract, and respiratory system by increasing the synthesis and activity of various anti-inflammatory agents. In 2013, peptides that prevent the formation of bacterial biofilms were discovered. So far, their development is at the preclinical stage.