The essence of the disease
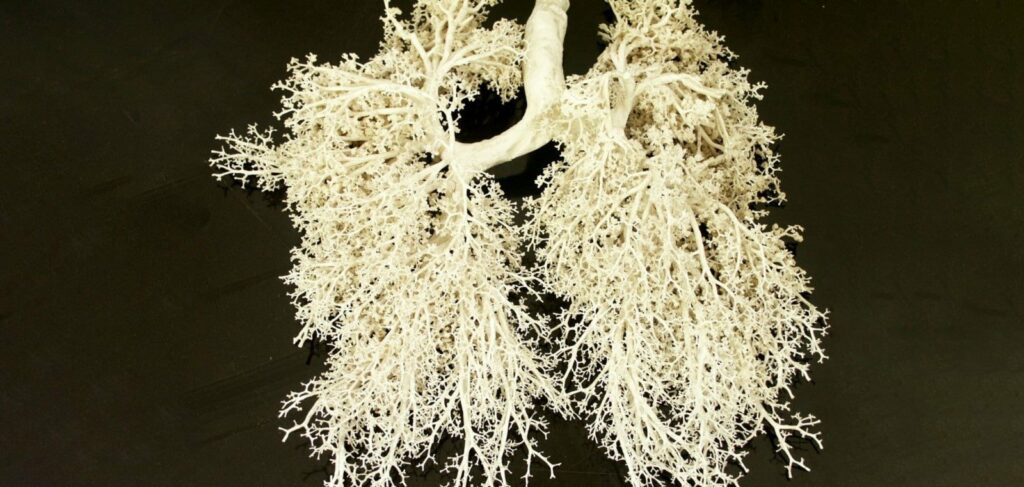
Bronchitis is an inflammation of large and small bronchi, which disrupts the normal function of the ciliated epithelium lining them from the inside. As a result, viscous sputum accumulates in the bronchi, which provokes coughing, and their mucous membrane swells, which makes breathing more difficult. In severe cases, the disease is complicated by obstruction, ie, violation of patency of the airways, or bronchospasm – a sharp narrowing of the lumen of the bronchi, caused by contraction of smooth muscle fibers of their walls.
There are two types of bronchitis: acute and chronic. Although their symptoms are often similar, each form of the disease has different causes and each has its own treatment methods.
Acute bronchitis is usually viral
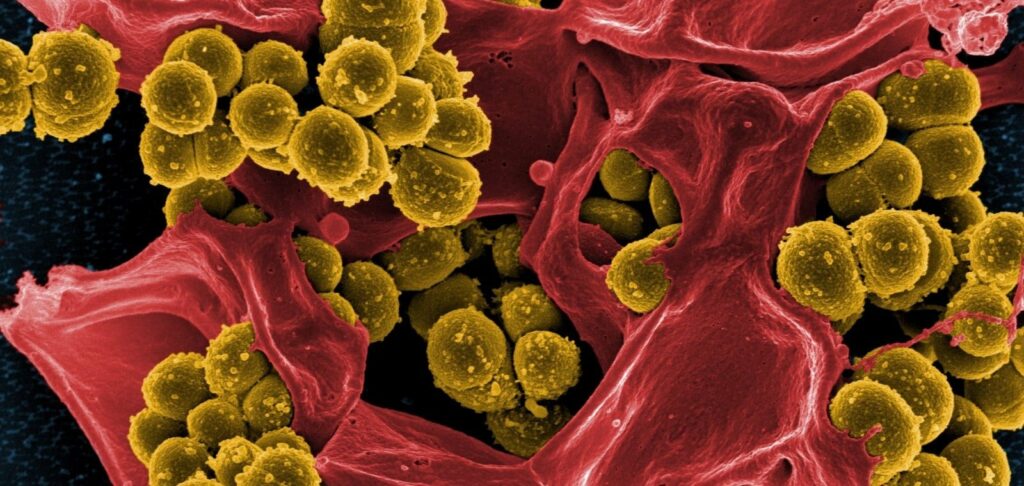
Each year, acute bronchitis affects approximately 5% of adults and 6% of children. In more than 90% of cases it occurs as a complication after upper respiratory tract infection caused by adeno-, coronaviruses, influenza, parainfluenza, respiratory syncytial virus, rhinovirus and others. In 10% of cases the culprits of bronchitis are atypical bacteria Bordetella pertussis, Chlamydophila pneumoniae and Mycoplasma pneumoniae.
The dominant symptom of acute bronchitis is a productive cough. Sometimes it is accompanied by fever, runny nose, nasal congestion, headache. Less often wheezing, shortness of breath, chest discomfort are observed. Acute bronchitis refers to self-limited diseases, which means that it eventually passes on its own. The associated cough lasts for 2-3 weeks. Since this disease is usually caused by viruses, antibiotics are not indicated in its uncomplicated course. Treatment should be aimed at alleviating the patient’s condition. Anti-inflammatory, antihistamine and antitussive drugs, antispasmodics, and expectorants to facilitate the expectoration of sputum will help.
However, many studies have questioned the effectiveness of cough medicines in children under six years of age.
According to experts, non-pharmacological measures, such as breathing exercises, special massage, and drinking plenty of water, which also helps to thin the mucus, may be much more effective.
Chronic bronchitis
Unlike acute bronchitis, chronic bronchitis involves irreversible changes in the mucous membrane and walls of the bronchial tree due to prolonged or constant irritation of the respiratory tract by infectious agents, tobacco smoke, dust and so on. It is said when a low-productive cough torments a person for at least three months a year for more than two years in a row. Symptoms of this disease may also include wheezing and shortness of breath, which increases with exercise and lack of oxygen. In chronic bronchitis, a particularly strong cough is often observed in the morning, immediately after waking up. The sputum is yellow or green in color. Sometimes small flecks of blood can be seen in it.
Most adult patients with chronic bronchitis are smokers and have chronic obstructive pulmonary disease (COPD) in addition to bronchial inflammation. In children, prolonged bronchitis is usually associated with an infection caused by Streptococcus pneumoniae, Haemophilus influenzae or Moraxella catarrhalis. Therefore, if they have a cough lasting more than 4 weeks, they are usually prescribed a course of antibacterial drugs after other diseases such as pneumonia or respiratory allergies have been ruled out.
Sometimes chronic bronchitis is a companion of bronchial asthma or is an occupational disease. People whose work is related to coal mining, grain processing, textile production, metal casting, and animal husbandry are at risk. Recently, chronic bronchitis has also been diagnosed quite often in residents of large cities, which is apparently due to air pollution in megacities.
Since chronic bronchitis is irreversible, the main goal of its therapy is to improve the patient’s quality of life, slow the progression of the disease and prevent complications. For this purpose, bronchodilators (they dilate the airways, relieving bronchospasm) and inhaled corticosteroids (reduce edema and inflammation of the epithelium) are used. Such drugs should be prescribed by a doctor, because it is very important to choose the optimal combination of drugs and their dosage to minimize the risk of side effects. In the exacerbation of chronic bronchitis, mucolytics help. Patients’ condition is also improved by physical therapy aimed at strengthening respiratory muscles and oxygen therapy.
Consultation with a primary care provider
Of course, the pharmacist cannot make a diagnosis, but he or she can help customers who come to the pharmacy with cough complaints to understand the causes of the disease, alleviate its symptoms, warn against incorrect treatment and, most importantly, advise them to see a doctor in time.
First of all, it should be remembered that the treatment of bronchitis does not require the use of antibiotics, except when the assumption of bacterial infection is confirmed not only clinically (persistent high body temperature, purulent sputum, signs of marked intoxication, rales in the bronchi on auscultation, etc.), but also laboratory data.
Before recommending a cough medicine, the pharmacist should find out the nature of the cough. A dry, tickling cough that occurs in response to throat discomfort usually occurs either at the beginning or at the end of an acute respiratory viral illness. It is associated with irritation of the mucous membrane of the throat, larynx and trachea by inflammation or mucus flowing down the back wall of the pharynx from the nose during a runny nose. Such a cough is not accompanied by the formation of sputum. It can be relieved by using throat sprays or sucking on lozenges with antiseptics, but in severe cases a person may need cough medicines that block the cough center in the brain. Such means relieve coughing attacks, which aggravate irritation and traumatize the inflamed surface of the mucous membrane of the lower respiratory tract.
Moist chest cough most often indicates precisely the development of bronchitis. Its main task is to clear the airways of sputum accumulated in them as a result of inflammation. However, because of its too thick and viscous consistency, this is not easy to achieve.
For non-productive coughs, the primary care provider may recommend expectorants, or mucolytics, which increase the evacuation function of the ciliated epithelium covering the bronchi, liquefy sputum and stimulate its discharge.
It is important to note that in dry cough expectorants will not only not relieve the person’s condition, but also serve as an additional irritant to the respiratory system. Conversely, with a wet cough, blocking the cough reflex with drugs of central action will lead to stagnation of sputum in the bronchi, increasing the risk of pneumonia.
Any cough in children under two years of age requires a doctor’s consultation. This is because the choice of drugs for this age group is very limited. In addition, small children can quickly develop pneumonia. Whooping cough is also a serious danger for them.
When counseling a client, the primary care provider should also clarify how long ago he or she had the cough. If it happened more than a month ago, you should see a doctor to rule out tuberculosis or asthma, confirm chronic bronchitis and get a treatment plan.
It is very important to make sure that the person suffering from a cough does not have:
- A fever above 38°C that persists for more than a week;
- chest pain with significant shortness of breath;
- severe weakness or excessive sweating;
- sputum with blood.
Any of these symptoms requires immediate medical consultation.