In clinical settings, the focus often heavily leans towards cancer treatment, neglecting nutritional care. This oversight can lead to severe consequences for patients.
The European Society for Clinical Nutrition and Metabolism (ESPEN) has established nutritional guidelines for cancer patients, but there’s a significant disconnect between these guidelines and their implementation in hospitals and clinics.
This issue is critical and demands immediate attention from healthcare providers, patients, and their families.
The Prevalence and Impact of Malnutrition in Cancer Patients
Malnutrition affects a significant proportion of cancer patients:
- Up to 75% of cancer patients experience some form of malnutrition [source]
- Malnutrition rates are higher in cancer populations than the general population
Types of Malnutrition in Cancer
There are two main types of malnutrition in cancer:
- Anorexia – lack of appetite leading to insufficient calorie/nutrient intake
- Cachexia – weight loss and muscle wasting despite adequate intake, due to abnormalities in metabolism caused by cancer
Consequences of Malnutrition
Malnutrition can negatively impact cancer patients in multiple ways:
- Increases toxicity of cancer treatments
- Reduces tolerance and compliance with treatments
- Diminishes response to therapies like chemotherapy
- Delays cancer treatment timelines
- Lowers quality of life
- Leads to higher cancer recurrence rates
- Worsens prognosis and survival rates
Types of Cancer with Greater Nutritional Impact
| Cancer Type | Nutritional Impact |
| Digestive (stomach, bowel, pancreatic) | Disrupts digestion & nutrient absorption |
| Head and neck | Difficulty eating & swallowing |
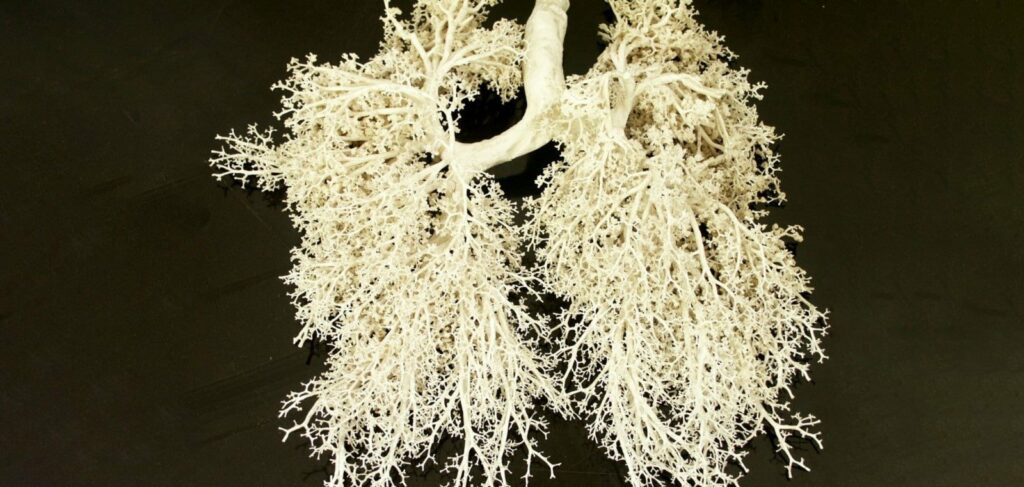
| Lung cancer | Distinct metabolic changes |
Addressing Malnutrition in Cancer Patients
- Early screening for malnutrition
- Personalized diet advice and nutritional counseling
- Oral nutrition supplements if needed
- Tube feeding or IV nutrition in severe malnutrition
Catching and correcting malnutrition early has significant benefits including:
- Improves ability to complete treatment protocols
- Reduces side effects and complications
- Enhances quality of life
- Could improve remission and survival odds
The inclusion of tailored medical nutrition therapy in cancer care plans is vital for combating malnutrition and supporting patients’ wellbeing and outcomes.

High Rates of Malnutrition in Cancer Patients Revealed in Recent Study
A sizable study published in 2022 in the journal Clinical Nutrition brought to light the widespread issue of malnutrition among cancer patients undergoing treatment.
The cross-sectional study analyzed 651 patients across 8 major cancer centers in the Netherlands. The patient sample included a diverse range of cancer types and treatment modalities.
Utilizing established nutritional screening tools designed specifically for cancer populations, the researchers found that 37% of patients were malnourished upon initial assessment.
This indicates that over one-third of cancer patients are starting treatment in an already-compromised nutritional state, putting them at high risk for further deterioration.
Perhaps even more alarming, the data showed that among this malnourished group, 80% had ongoing weight loss apparent at the 6-month mark of analysis. The median weight change was a loss of 7.1% body weight over just a half-year into cancer therapy. Unintended weight loss of 5% is considered clinically significant.
Muscle wasting was also noted in these patients. Clearly a high percentage of patients were experiencing progression of malnutrition while actively undergoing anticancer treatments.
Weight loss and dwindling muscle mass denotes the body breaking down its own tissues to fuel basal metabolism. This not only affects quality of life but can directly impair tolerance and response to therapies.
The patient subset that was well-nourished at baseline actually saw less weight fluctuations, pointing to the protective power of nutrition. However, without screening, malnutrition can be easily overlooked until symptoms like rapid weight loss arise.
At minimum, nutrition guidelines in oncology call for protein intakes of ≥1.0g/kg/day to maintain muscle mass. Yet the current data indicates patients struggle to meet these targets without intervention.
The researchers conclude proactive nutrition care models should be integrated alongside cancer treatment protocols to curb the development and worsening of malnutrition during the treatment journey.

Significance and Takeaways
The recent study highlighting malnutrition in cancer patients is a wake-up call for the medical community and patient care. It reveals that up to 70% of cancer patients suffer from malnutrition, often losing weight during treatment.
This alarming finding emphasizes the need for early nutritional intervention as a critical part of cancer care.
Early nutritional intervention goes beyond being a supplement to cancer treatment. It’s a key factor that affects treatment effectiveness, patient quality of life, and survival rates. Proper nutrition can counter muscle wasting, a common issue in malnourished cancer patients, enhancing their strength and resilience.
It also bolsters the immune system, crucial for fighting cancer and recovering from treatments.
This study suggests the need to revise clinical practice guidelines to include routine malnutrition screening and integrate nutritional support into cancer treatment protocols.
Such guidelines may recommend specialized nutritional products and diets, like those offered by Priora Nutrition, which develops enteral feeding mixtures in line with ESPEN recommendations.
Their specialized diets, including the Priora Nutrition Onco Diet, are designed to meet cancer patients’ specific nutritional needs, supporting their health and recovery.
Incorporating these specialized diets, such as the Priora Nutrition Onco Diet, into cancer care can be a significant step in combating malnutrition. This diet, developed according to ESPEN guidelines, provides essential nutrients to patients undergoing cancer treatment, potentially improving patient outcomes.

Ways Families Can Help Support the Nutritional Needs of Relatives Being Treated for Cancer
When a loved one is going through cancer treatment, it can be very difficult for family members who want to help but aren’t sure what to do. Proper nutrition plays a vital role in supporting health and recovery, but cancer and its treatments can make eating a challenge. Families can provide practical, nutritional support in the following ways:
Meal Planning and Preparation
- Plan meals and snacks around the patient’s food preferences and any treatment-related dietary restrictions
- Prepare nutrient-dense meals and snacks that include:
- Lean protein sources like poultry, fish, eggs, beans, tofu
- Whole grains like brown rice, quinoa, whole wheat pasta
- Fruits and vegetables, especially dark leafy greens
- Healthy fats from nuts, seeds, olive oil, avocado
- Try batch cooking things like soups, stews, and casseroles so there are leftovers to heat and eat later
Consulting Healthcare Providers
- Talk to doctors, nurses, and registered dietitians about the patient’s nutritional needs
- Ask for nutritional supplements or specialized nutrition advice if the patient is struggling to eat or maintain weight
- Get recommendations on hydration needs and optimal ways to meet daily fluid intake

Specialized Nutritional Support
- Incorporate nutrient-dense shakes or drinks recommended by healthcare providers to supplement meals
- Use products designed specifically for cancer patients like:
- Priora Nutrition Onco Diet – formulated with a balanced mix of nutrients to address malnutrition
- Drink mixes with extra protein and calories
- Probiotic supplements to support gut health
Eating well through cancer treatment can be hugely beneficial but challenging. By taking an active role in meal planning, preparation, and seeking expert guidance, families can provide vital nutritional support during this difficult time.
Conclusion
The data shows us that malnutrition reaches crisis levels in cancer populations, yet remains overlooked and undertreated. With up to 70% of patients malnourished and ongoing weight loss undermining treatment, nutrition care in oncology is no longer optional – it is essential for managing symptoms, enhancing quality of life, improving outcomes, and saving lives.
Specialized nutrition is proven to help cancer patients increase calorie, protein and micronutrient intake, minimize weight fluctuations, tolerate treatments better, avoid hospitalizations, and more.
Optimal nutrition empowers patients with energy and strength to keep fighting. Ensuring adequate intake means supporting the whole patient – mind, body and spirit.
Call to Action
We call on patients, caregivers, and providers to collectively prioritize anti-cancer nutrition at both individual and institutional levels. As a community, we must drive change through open dialogue and concrete action.
Patients and Caregivers:
- Speak up in asking about nutrition care options
- Track weight during treatment; flag unintended losses
- Incorporate nutrient-dense meals and snacks
- Seek medical nutrition if needed to meet guidelines
Providers and Cancer Centers:
- Implement mandatory nutrition screening at diagnosis
- Refer patients to expert dietitians at first signs of weight loss
- Integrate oral nutrition supplements into care plans
- Expand nutritional services and educational resources
Join us in making nutrition care a standard component of quality cancer care worldwide. Together, we can tackle malnutrition to transform patient experiences and save lives.