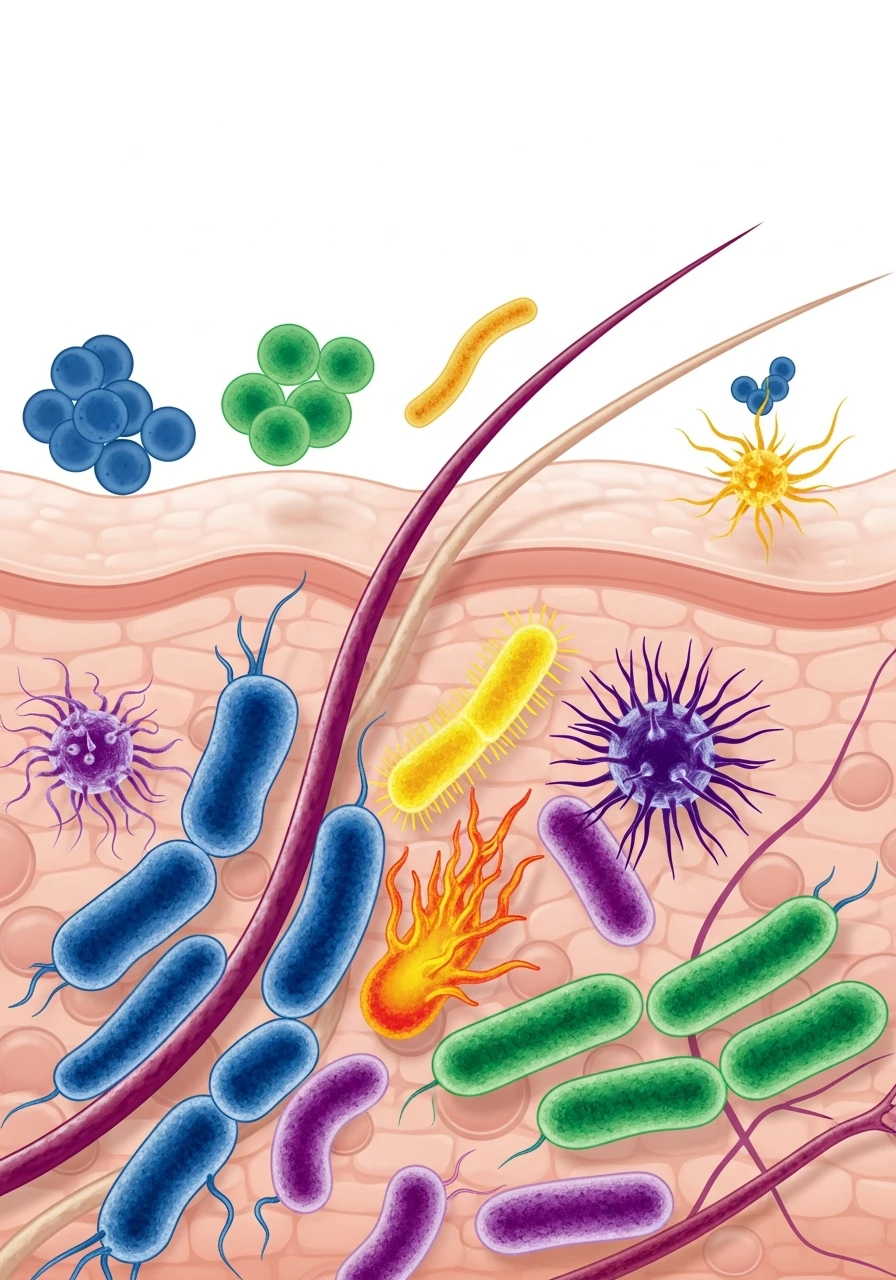
The skin microbiome consists of thousands of microorganisms that live on our skin and help protect against pathogens, regulate inflammation, and even influence barrier functions. Temperature, humidity, and sunlight change with the seasons—and the microbiome changes as well.
In this article, we explore how different seasons affect the skin microflora and what role skincare and nutraceuticals can play.

Skin microbiome: a brief overview
The skin microbiome consists of bacteria, fungi, viruses, and mites that live in balance with our body. Their balance determines:
-
the skin’s barrier properties;
-
the level of local inflammation;
-
the risk of infections and flare-ups of chronic dermatoses.
Seasonal environmental changes affect:
-
the composition of dominant species;
-
the activity of sebaceous and sweat glands;
-
skin moisture levels.
Table 1. Seasonal factors affecting the skin microbiome
| Seasonal factor | Potential impact on the microbiome | Clinical consequences |
|---|---|---|
| High humidity | growth of certain fungal species | exacerbation of seborrheic dermatitis |
| High temperature | changes in bacterial community composition | increased oiliness, acne |
| Low humidity | reduced microbiome diversity | dryness, flaking, irritation |
| UV radiation | effects on microbial populations and skin immunity | photoaging, pigmentation changes |
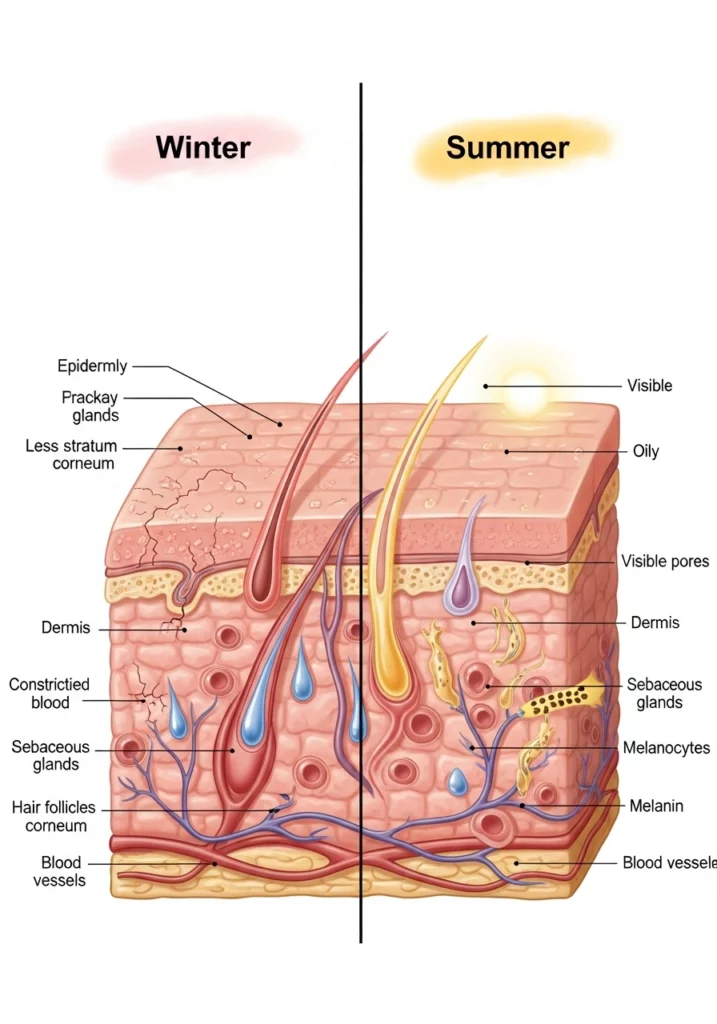
During the warm season (spring–summer), increased sebaceous gland activity, sweating, and ultraviolet exposure are more common. In the cold season (autumn–winter), dryness, reduced microbiome diversity, and a tendency toward irritation prevail.
Summer: temperature, humidity, and sunlight
During the summer:
-
environmental temperature and humidity increase;
-
sweating increases;
-
certain bacteria and fungi become more active.
This may lead to:
-
acne flare-ups;
-
seborrheic dermatitis;
-
fungal infections in skin folds.
At the same time, moderate UV exposure may have anti-inflammatory effects, while excessive exposure can damage the barrier and shift microbial communities in an undesirable direction.
Winter: dry air and the skin barrier
In winter, air humidity decreases and temperature fluctuations become more frequent, which:
-
reduces microbiome diversity;
-
increases skin sensitivity;
-
may contribute to flare-ups of atopic dermatitis, xerosis, and irritation.
Table 2. Examples of dermatological conditions associated with seasonality
| Condition | More likely to worsen when | Possible link to the microbiome |
|---|---|---|
| Acne | spring–summer | changes in bacterial composition and sebum |
| Seborrheic dermatitis | autumn–winter, spring | yeasts and barrier alterations |
| Atopic dermatitis | winter | dryness, reduced flora diversity |
| Fungal infections | summer | heat, humidity |
A seasonal approach to skincare is important: the “same” routine year-round often does not work.

How to prepare the skin and body for winter
-
With increased dryness—focus on barrier-repair creams, emollients, and minimalist formulations.
-
Avoid overly aggressive cleansing and frequent peels.
-
Support nutrient status: omega-3 PUFAs, vitamin D, antioxidants (vitamins C, E, polyphenols).
How to prepare for summer
-
Lighter product textures while maintaining barrier support (niacinamide, light emollients).
-
Regular use of sunscreen.
-
Control sweating without excessive drying (caution with alcohol-based sprays).
-
Possible use of probiotic/postbiotic topical products that support microbiome balance.

The role of nutraceuticals
Oral nutraceuticals do not directly “control” the skin microbiome, but they can:
-
affect systemic inflammation (omega-3, polyphenols);
-
support gut microbiome health (probiotics, prebiotics, postbiotics), which is linked to the gut–skin axis;
-
improve antioxidant status (vitamins C, E, carotenoids).
Questions and answers
Are separate “probiotics for the skin” necessary?
Oral probiotics primarily affect the gut, but through systemic mechanisms they can also influence the skin. Topical “probiotic” products are often postbiotics or bacterial fragments rather than live microorganisms.
Is it necessary to change skincare every season?
Yes, but not always radically. At a minimum—adjust textures (richer in winter, lighter in summer) and cleansing intensity.
Is there a reason to change the diet?
Yes, especially by increasing vegetables, fiber, omega-3 intake, and reducing excess sugar and ultra-processed foods.
Can the skin be “conditioned” for summer or winter?
Partially—through gradual changes, but extremes (sudden shifts, aggressive peels) usually worsen the condition.
Conclusions
The skin microbiome dynamically responds to seasonal changes in temperature, humidity, and solar radiation. Seasonally adapted skincare (adjusting textures, cleansing frequency, exfoliation intensity, and level of protection) together with a supportive nutraceutical approach (omega-3s, antioxidants, microbiome-supporting components) helps reduce the risk of dermatosis flare-ups and maintain healthy skin throughout the year.
References
-
Belkaid Y., Segre J.A. Skin microbiota and immunity.
-
Sanford J.A., Gallo R.L. Functions of the skin microbiota in health and disease.
-
Byrd A.L. et al. The human skin microbiome.
-
Dréno B. et al. Microbiome in dermatology: seasonal aspects.