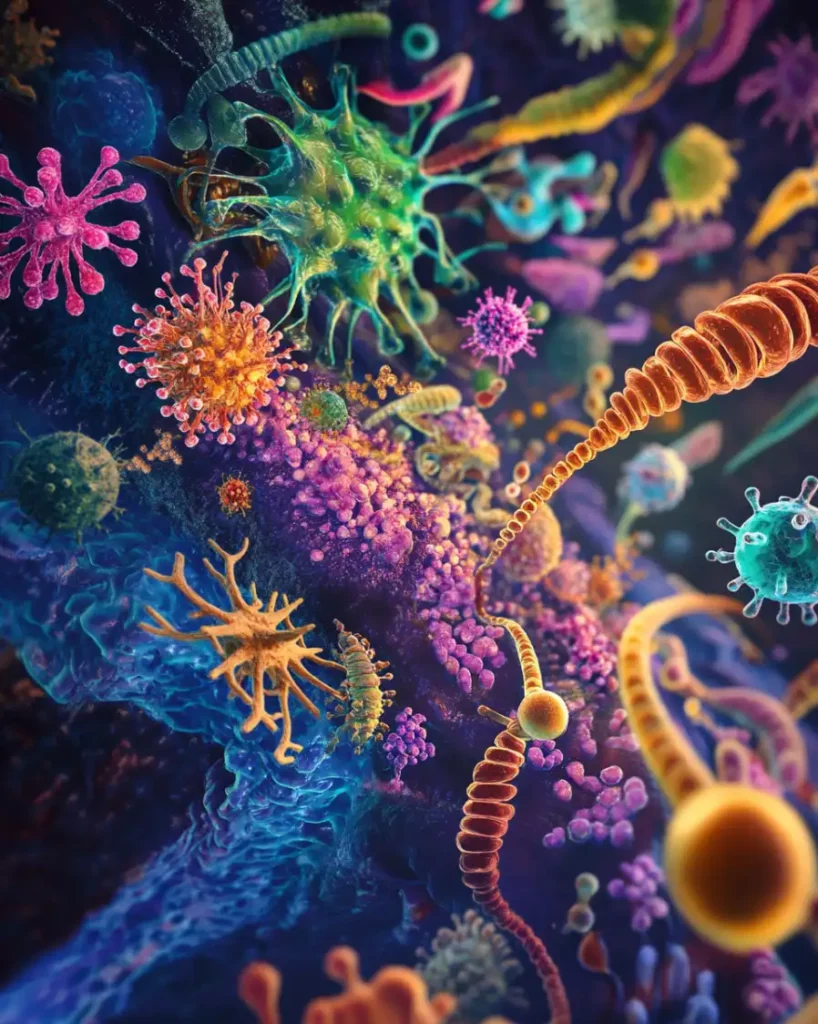
The human microbiome, which includes bacteria, viruses, fungi and archaea, has received increased attention in recent years because of its enormous impact on various aspects of health.
These microorganisms, predominantly inhabiting the gut, outnumber the cells of the human body and play a key role in regulating a multitude of physiological processes.

A healthy microbiome contributes to a strong immune system, optimal metabolic function and stable mental health, while its imbalance, known as dysbiosis, can lead to a range of diseases.
In this article, we detail how the microbiome affects the immune system, mental health, and metabolism based on the latest scientific research, and discuss the promise of microbiology-based personalized medicine.

The microbiome and the immune system
The role of the microbiome in the development of immunity
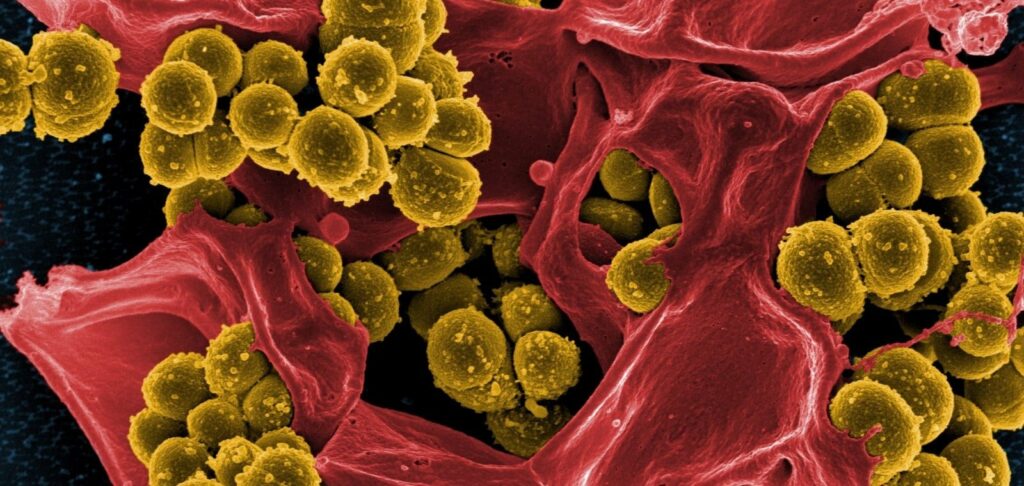
The human immune system and the microbiome maintain a symbiotic relationship.
Gut bacteria participate in a dynamic interaction with immune cells through complex signaling pathways, contributing to both innate and adaptive immunity.
For example, gut bacteria stimulate the production of cytokines and antibodies important for regulating immune processes.
Case Study Example:
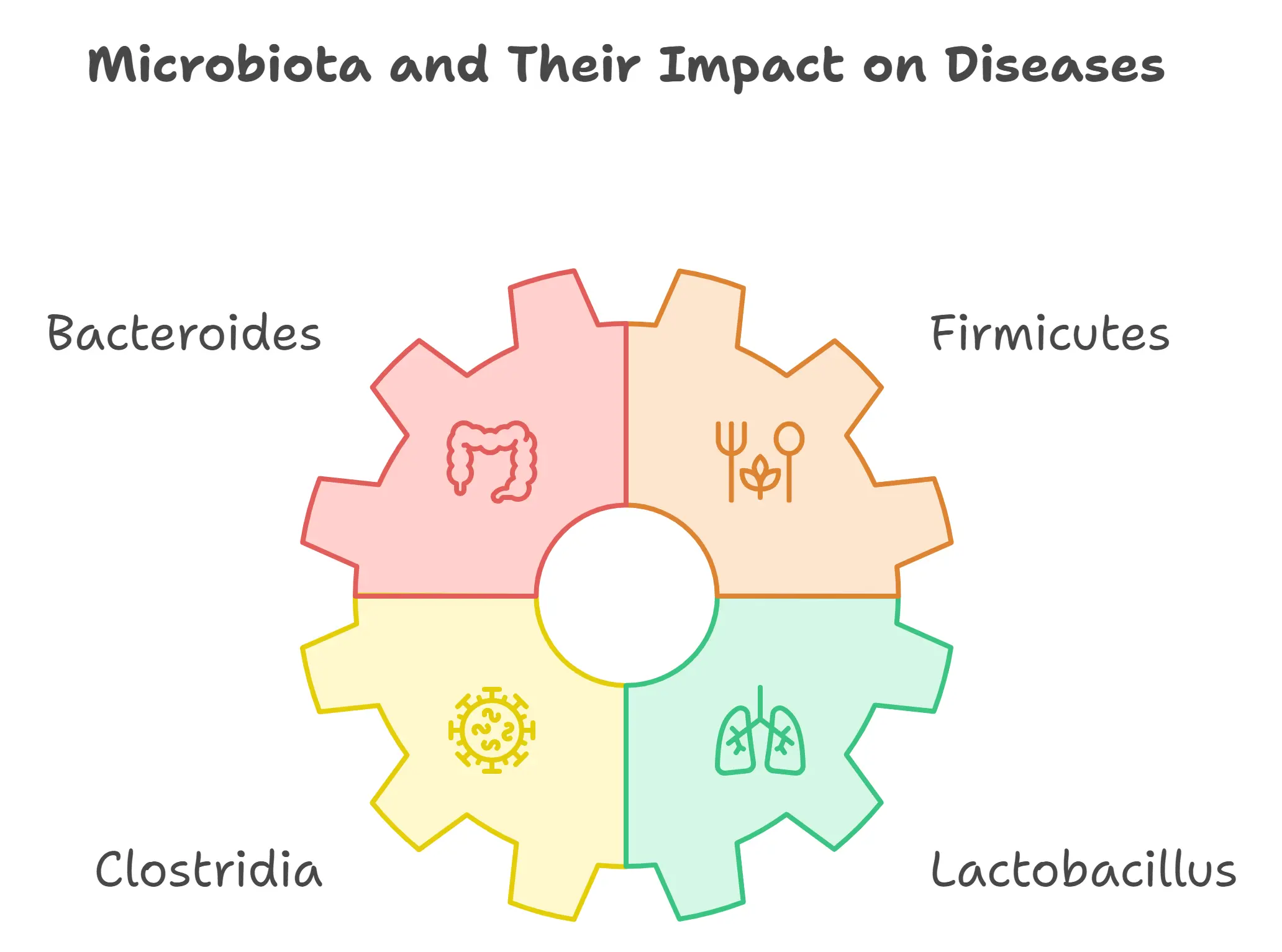
A 2017 study conducted at the University of California found that the presence of bacteria of the genus Bacteroides and Firmicutes in the gut enhances the immune response to pathogens.
These microorganisms not only protect the body from infections, but also help the immune system distinguish safe substances from potential threats, which reduces the risk of autoimmune diseases such as rheumatoid arthritis and lupus.

Dysbiosis and its consequences
Dysbiosis, an imbalance of the gut microbiota, is associated with increased susceptibility to inflammatory diseases.
People with conditions such as Crohn’s disease and ulcerative colitis have a significant decrease in microbiota diversity, which is associated with increased inflammation.
Extended Table 1: Impact of dysbiosis on the immune system
| Type of Microbiota | Associated Diseases | Mechanism of Action |
|---|---|---|
| Bacteroides | Autoimmune diseases | Modulation of inflammatory processes |
| Firmicutes | Allergies | Regulation of immune molecule production |
| Clostridia | Chronic inflammatory diseases | Maintenance of intestinal barrier functions |
| Lactobacillus | Respiratory infections | Immunomodulation and competition with pathogens |
Additional data
Current research shows that early exposure to microbes (e.g., through natural childbirth and breastfeeding) is critical for proper immune system development.
Infants born by cesarean section or formula-fed have a different microbiota composition, which may explain the higher prevalence of allergies and asthma in these groups.

The microbiome and mental health
The gut-brain axis: two-way communication
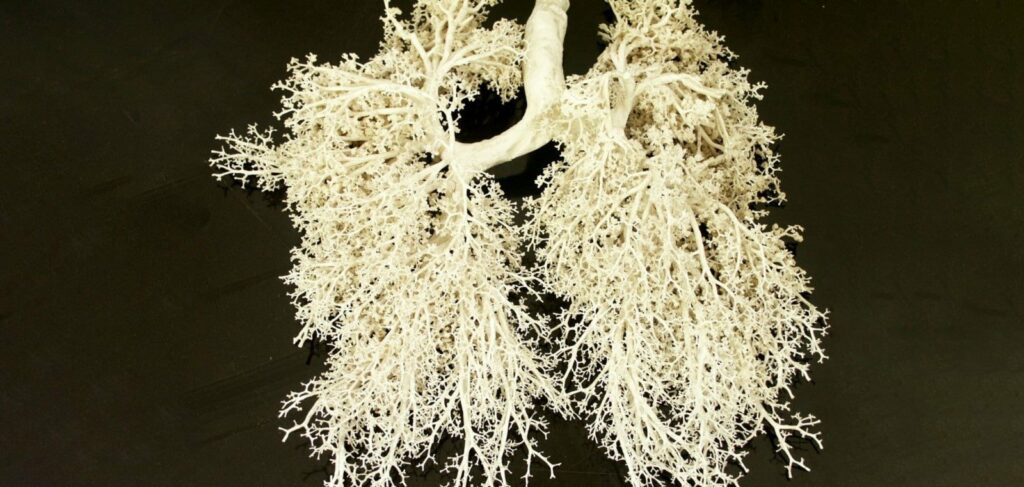
The gut-brain axis is a two-way communication system between the gut microbiome and the central nervous system (CNS).

Gut bacteria produce neuroactive compounds such as serotonin, dopamine, and gamma-aminobutyric acid (GABA) that directly affect brain function and mood regulation.

A 2019 study from the University of Oxford found that probiotics containing Bifidobacterium longum improved mental health in 70% of patients with clinical depression, reducing anxiety and improving cognitive function .
This provides promising evidence that targeting the microbiome may be a new approach to the treatment of psychiatric disorders.
Expanded Table 2: Impact of microbiota on mental health
| Type of Microbes | Connection to Mental Health | Role in the “Gut-Brain Axis” |
|---|---|---|
| Bifidobacterium longum | Reduces anxiety and depression | Production of serotonin and GABA |
| Lactobacillus rhamnosus | Improves stress response | Modulates the hypothalamic-pituitary-adrenal axis and cortisol levels |
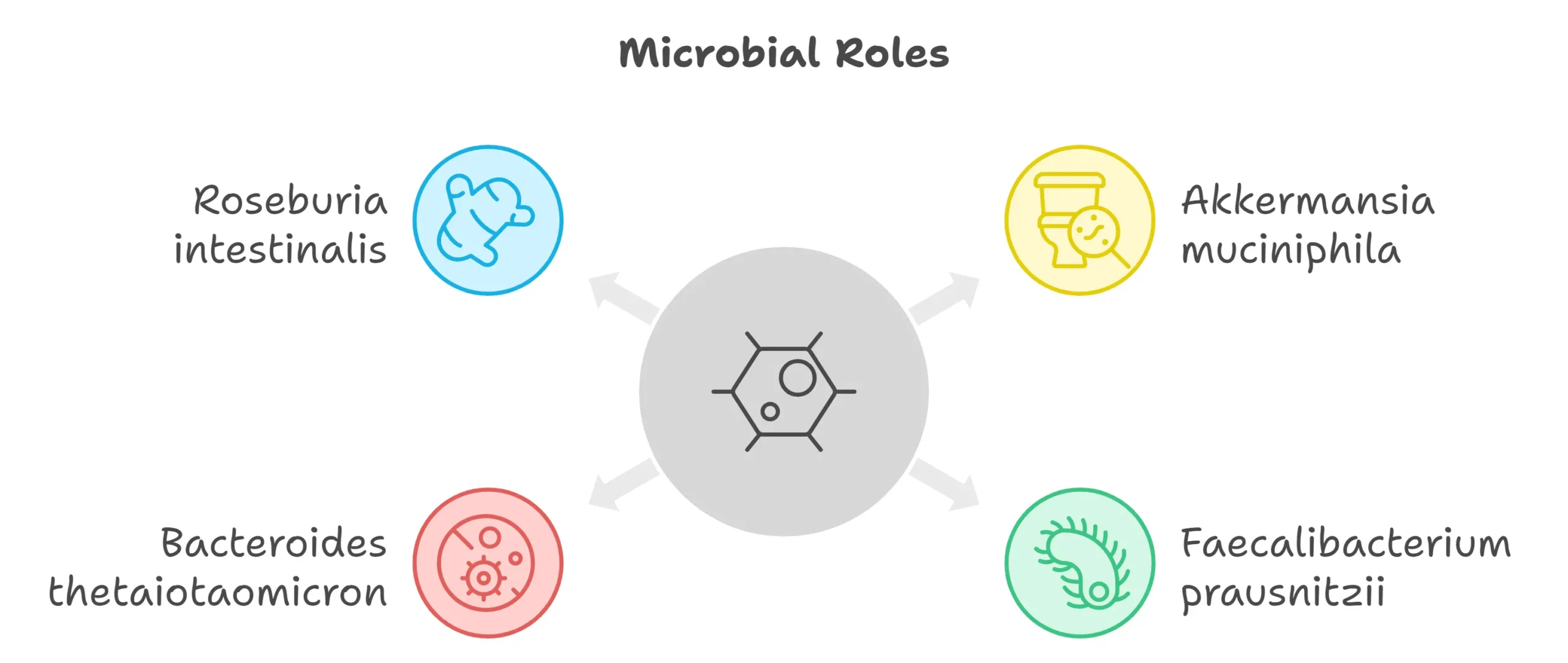
| Faecalibacterium prausnitzii | Enhances cognitive functions | Anti-inflammatory effects on the central nervous system |
Probiotics and mental health
Studies have shown that probiotics and prebiotics (substances that nourish beneficial gut bacteria) can have therapeutic effects on mental health.
A 2020 meta-analysis showed that people with mild to moderate depression showed significant improvement after taking probiotics containing strains of Lactobacillus and Bifidobacterium.

Microbiome and metabolism
Role of microbiota in metabolic processes
The gut microbiota has a significant impact on metabolism by assisting in the breakdown of dietary fiber into short-chain fatty acids (SCFAs), which regulate glucose and lipid metabolism.
Moreover, microbiota diversity influences nutrient absorption, vitamin synthesis and energy balance.
A 2020 study conducted at Cornell University found that obese people had lower levels of Akkermansia muciniphila, a bacterium associated with improved lipid metabolism and glucose homeostasis.
It was found that taking Akkermansia in obese people promoted weight loss and improved insulin sensitivity .
Expanded Table 3: Role of microbiota in metabolism
Additional data
Dysbiosis has been linked to the development of obesity, type 2 diabetes and metabolic syndrome.
Obese people are more likely to have bacteria of the genus Firmicutes, while lean people have more bacteria of the genus Bacteroidetes.
This change in the microbiota is thought to alter the way energy is extracted from food, which contributes to weight gain.
Conclusion
The human microbiome is a complex ecosystem that plays an important role in the regulation of the immune system, mental health, and metabolism.
A healthy microbiome supports the overall health of the body, while dysbiosis contributes to a wide range of chronic diseases such as autoimmune disorders, depression and metabolic disorders.
Maintaining a healthy microbiome requires eating a varied and balanced diet that includes fiber, prebiotics and probiotics, and minimizing the use of antibiotics without a medical indication.
New research suggests that personalized microbiome therapies may form the basis of future medical approaches, offering tailored solutions to improve health outcomes.
The potential for microbiome interventions in both preventive and therapeutic medicine is enormous.
As our understanding of microbiological science deepens, it is expected that in the next decade we will see significant breakthroughs in this field that will radically change approaches to treatment and health management.