Have you ever noticed small, rough bumps on your arms or legs that resemble goosebumps or chicken skin?
If so, you may have keratosis pilaris (KP), a common and harmless skin condition that affects up to 50-80% of adolescents and 40% of adults.
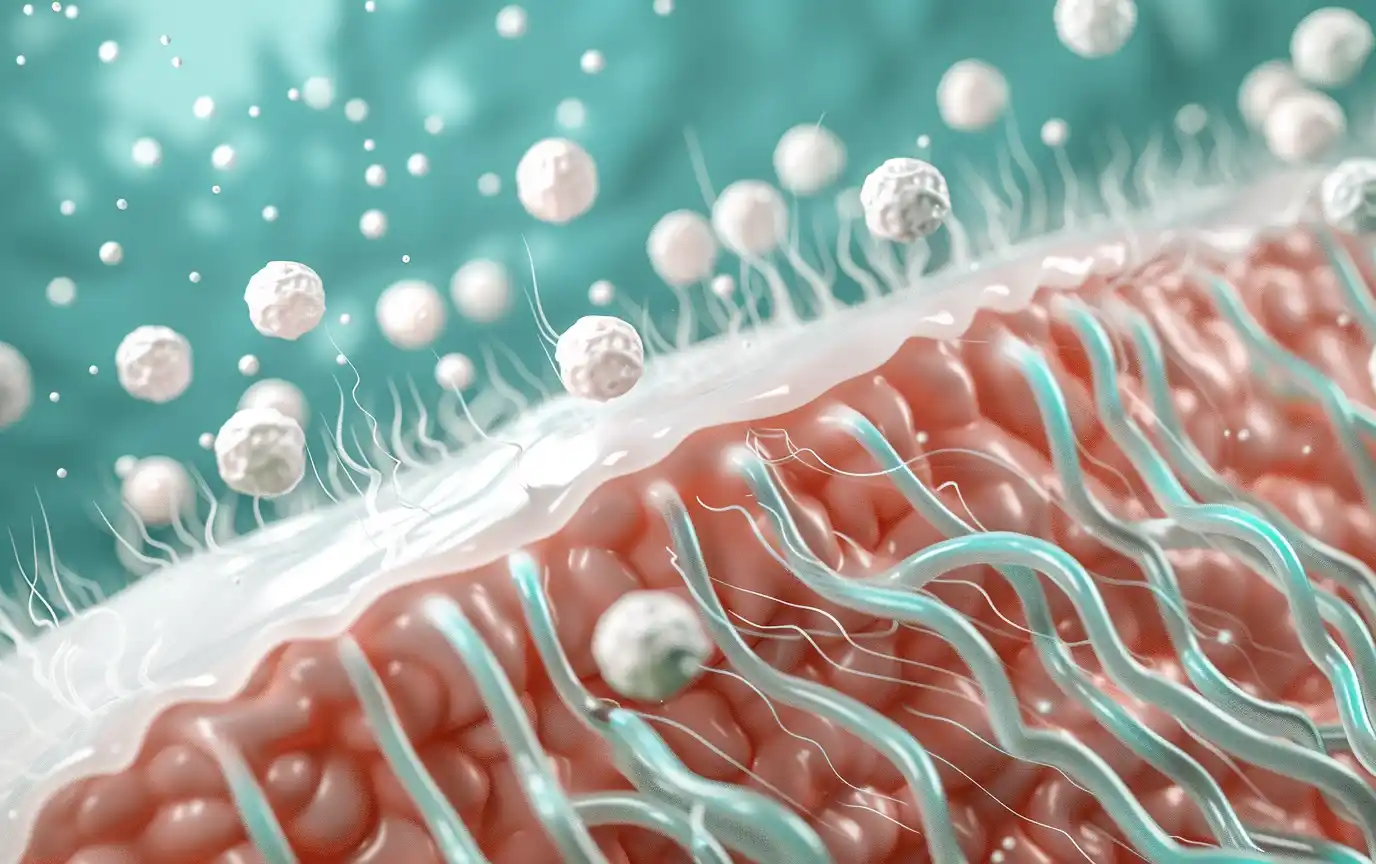
Keratosis pilaris occurs when keratin, a protein that protects the skin, builds up and clogs hair follicles, resulting in the characteristic bumpy appearance.
While keratosis pilaris is not painful or contagious, it can be a cosmetic concern for some individuals.
As a doctor, I’m here to provide you with friendly information to understand the causes, symptoms, and treatment options for keratosis pilaris.
You’ll be equipped with the knowledge and tools to manage this stubborn but manageable skin condition.

What is Keratosis Pilaris?
What Causes Those Annoying Goosebumps?
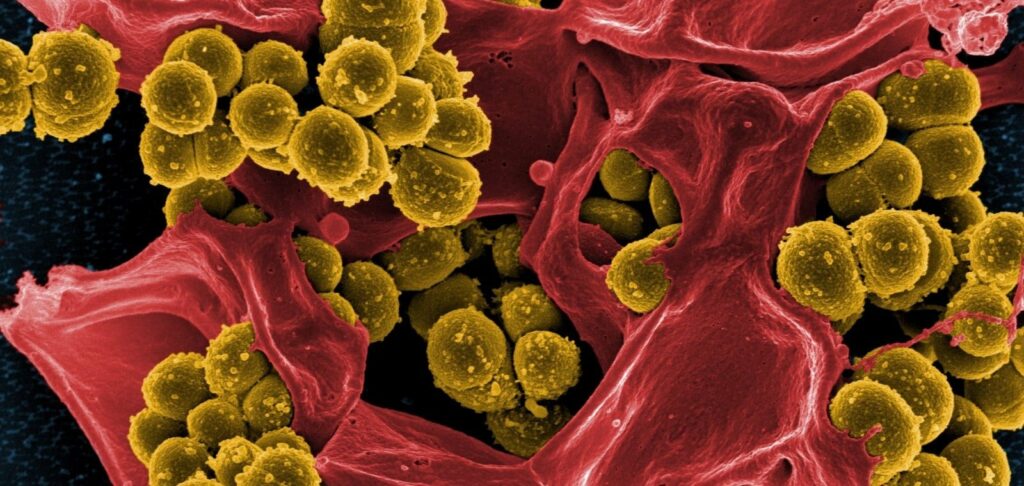
Keratosis pilaris develops when keratin, a hard protein that protects the skin from infections and other harmful substances, accumulates and forms a plug that blocks the opening of the hair follicle.
Normally, keratin is shed gradually from the skin’s surface, but in individuals with keratosis pilaris, this process is disrupted, leading to the characteristic rough, bumpy texture of the skin.
It’s important to note that while keratosis pilaris may be unsightly, it is a benign condition that does not pose any health risks.
The bumps, which can be skin-colored, red, or brown, are not painful or itchy for most people.
However, some individuals may experience mild itching or dryness, especially during the winter months when the air is less humid.
Keratosis pilaris most commonly affects the outer upper arms, thighs, cheeks, and buttocks, but it can appear on any area of the body with hair follicles, except for the palms and soles.
The condition is often referred to as “chicken skin” due to its goosebump-like appearance.

Who Gets Keratosis Pilaris?
Several factors can increase your likelihood of developing keratosis pilaris, including:
- Genetics: Keratosis pilaris tends to run in families, suggesting that certain genetic traits may predispose individuals to the condition.
- Age: The condition is more common in children and adolescents, with up to 50-80% of teenagers being affected. Keratosis pilaris often improves with age and may clear up by the time an individual reaches their 30’s.
- Dry skin: Individuals with dry skin or eczema (atopic dermatitis) are more prone to developing keratosis pilaris.
- Seasonal changes: Keratosis pilaris tends to worsen during the dry, cold winter months and improve in the summer when humidity levels are higher.
- Hormonal fluctuations: Hormonal changes during pregnancy can trigger or exacerbate keratosis pilaris.
While the exact cause of keratosis pilaris is not fully understood, researchers believe that a combination of genetic, environmental, and hormonal factors contribute to the development of the condition.
Some studies have also suggested a link between keratosis pilaris and vitamin A deficiency, although more research is needed to confirm this association.
It’s important to remember that keratosis pilaris is a very common condition, affecting a significant portion of the population.
If you have keratosis pilaris, you are not alone, and there are many treatment options available to help manage the symptoms and improve the appearance of your skin.
In the next section, we’ll explore the signs and symptoms of keratosis pilaris in more detail and discuss when it’s time to see a dermatologist for an accurate diagnosis and personalized treatment plan.

Keratosis Pilaris Symptoms
How to Identify Keratosis Pilaris
Keratosis pilaris is characterized by its distinctive appearance, which is often described as “goosebumps,” “chicken skin,” or “sandpaper-like” texture.
The bumps are typically skin-colored, white, or slightly red, and they may be more noticeable when the skin is dry.
In some cases, the bumps can become inflamed or have a pimple-like appearance.
The most common areas affected by keratosis pilaris include:
- Keratosis pilaris on arms: The upper outer arms are the most frequently affected area, with bumps often appearing on the back of the arms.
- Keratosis pilaris on legs / thighs: Bumps can also appear on the thighs, particularly the front and outer aspects of the upper legs.
- Keratosis pilaris on cheeks / face: Some individuals may develop keratosis pilaris on their cheeks or face, which can be mistaken for acne.
- Keratosis pilaris on buttocks: The buttocks can also be affected by keratosis pilaris, with bumps appearing on the upper and outer regions.
In addition to the characteristic bumps, some individuals with keratosis pilaris may experience other symptoms, such as:
- Redness: The bumps may be surrounded by mild redness or inflammation, especially if they have been scratched or irritated.
- Itchiness: While keratosis pilaris is not typically itchy, some people may experience mild itching, particularly when the skin is very dry.
It’s important to note that the severity of keratosis pilaris can vary from person to person, with some individuals having only a few scattered bumps and others experiencing more extensive involvement.

Is it Keratosis Pilaris or Something Else?
While keratosis pilaris has a distinct appearance, there are several other skin conditions that can cause similar bumps or rashes.
Some of these conditions include:
- Eczema (atopic dermatitis): Eczema is a chronic skin condition that causes dry, itchy, and inflamed skin. It can sometimes resemble keratosis pilaris, but eczema tends to be more itchy and may cause the skin to crack or ooze.
- Folliculitis: Folliculitis is an inflammation of the hair follicles, often caused by bacterial or fungal infections. It can cause red, itchy, or painful bumps that may be filled with pus.
Unlike keratosis pilaris, folliculitis bumps are usually more scattered and not as symmetrical.
- Acne: Acne is a common skin condition that occurs when hair follicles become clogged with oil and dead skin cells.
While acne can cause bumps and redness similar to keratosis pilaris, it typically affects the face, chest, and back, and the bumps may be accompanied by blackheads, whiteheads, or cysts.
If you’re unsure whether your bumps are caused by keratosis pilaris or another skin condition, it’s essential to consult with a dermatologist for an accurate diagnosis.

A dermatologist can examine your skin, assess your medical history, and perform any necessary tests to determine the underlying cause of your symptoms.
An accurate diagnosis is crucial for developing an effective treatment plan, as different skin conditions may require different approaches.
In some cases, what appears to be keratosis pilaris may be a sign of an underlying medical condition, such as an endocrine disorder or vitamin deficiency.

Treating Keratosis Pilaris
Over-the-Counter Keratosis Pilaris Treatments
While there is no cure for keratosis pilaris, several over-the-counter treatments can help manage the symptoms and improve the appearance of the skin.
The key to treating keratosis pilaris is a combination of gentle exfoliation and consistent moisturization.
Here are some recommended over-the-counter products:
- Moisturizers with ceramides, urea, or lactic acid: Look for moisturizers that contain ingredients like ceramides, which help to strengthen the skin’s barrier; urea, which softens and hydrates the skin; or lactic acid, an alpha-hydroxy acid (AHA) that gently exfoliates and moisturizes.
These ingredients can help to loosen and remove the keratin plugs that cause the bumps in keratosis pilaris.
Consider Cetaphil from Galderma, or Lacera from Schonen
- Gentle exfoliating body washes/scrubs with salicylic acid or glycolic acid: Exfoliation helps to remove dead skin cells and unclog hair follicles. Choose body washes or scrubs that contain salicylic acid, a beta-hydroxy acid (BHA) that penetrates the hair follicles and dissolves keratin plugs, or glycolic acid, an AHA that helps to smooth and even out the skin’s texture.
Be sure to use these products gently and avoid harsh scrubbing, which can irritate the skin.
- Fragrance-free cleansers and creams: Opt for gentle, fragrance-free cleansers and creams to avoid further irritation of the skin. Look for products that are labeled as “non-comedogenic,” meaning they won’t clog your pores.
When treating keratosis pilaris, it’s essential to be consistent with your skincare routine. Gentle exfoliation and regular moisturization can help to improve the texture and appearance of the skin over time.
However, it’s important to be patient, as it may take several weeks to a few months to see significant improvement.

Prescription Treatments for Keratosis Pilaris
In some cases, over-the-counter treatments may not be enough to manage keratosis pilaris symptoms.
If your condition is severe or not responding to self-care measures, your dermatologist may recommend prescription treatments, such as:
- Topical retinoids: Retinoids, which are derived from vitamin A, can help to unclog hair follicles and promote cell turnover.
Prescription-strength topical retinoids, such as tretinoin or tazarotene, may be more effective than over-the-counter retinol products.
However, these medications can cause skin irritation, redness, and dryness, so they should be used under the guidance of a dermatologist.
- Vitamin D creams: Topical vitamin D creams, such as calcipotriene, have been shown to improve the appearance of keratosis pilaris bumps.
These creams work by slowing down the growth of skin cells and reducing inflammation.
- Oral retinoids: In severe cases of keratosis pilaris that do not respond to topical treatments, oral retinoids, such as isotretinoin, may be prescribed.
These medications are typically reserved for short-term use due to potential side effects, such as dry skin, chapped lips, and sun sensitivity.
If you have persistent or severe keratosis pilaris, it’s important to consult with a dermatologist to determine the best course of treatment for your individual needs (keratosis pilaris prescription medication).
Your dermatologist can assess the severity of your condition and recommend the most appropriate prescription treatments.

Home Remedies for Keratosis Pilaris
In addition to over-the-counter and prescription treatments, there are several home remedies that may help to alleviate keratosis pilaris symptoms.
While the evidence supporting these remedies is limited, they are generally low-risk and may be worth trying in conjunction with other treatments.
Some popular home remedies include:
- Dry brushing: Gently brushing the affected areas with a soft-bristled brush before showering can help to exfoliate the skin and unclog hair follicles. Be sure to use light pressure and avoid brushing too harshly, as this can irritate the skin.
- Oatmeal baths: Adding colloidal oatmeal to your bathwater can help to soothe and moisturize the skin. Oatmeal has anti-inflammatory properties and can help to relieve itching and irritation associated with keratosis pilaris.
- Coconut oil: Applying coconut oil to the affected areas may help to moisturize and soften the skin. Coconut oil contains lauric acid, which has antimicrobial properties and may help to reduce inflammation.
However, be cautious when using coconut oil on the face, as it may clog pores in some individuals.
- Humidifier: Using a humidifier in your home can help to add moisture to the air, which may prevent the skin from becoming too dry. Dry skin can exacerbate keratosis pilaris symptoms, so maintaining proper humidity levels can be beneficial.
It’s important to note that while these home remedies may provide some relief, they should not be used as a substitute for medical treatment in severe cases.
If your keratosis pilaris symptoms persist or worsen despite self-care measures, be sure to consult with a dermatologist for further guidance.

Living Well with Keratosis Pilaris
Lifestyle Tips for Managing Keratosis Pilaris
In addition to medical treatments and home remedies, making certain lifestyle changes can help to manage keratosis pilaris symptoms and prevent flare-ups. Here are some tips to keep in mind:
- Wear loose clothing: Tight clothing can irritate the skin and exacerbate keratosis pilaris bumps. Opt for loose, breathable fabrics like cotton to minimize friction and allow your skin to breathe.
- Use lukewarm water: Hot water can strip the skin of its natural oils, leading to dryness and irritation. When showering or bathing, use lukewarm water and limit your time to 10 minutes or less.
- Avoid irritants like hot tubs: Hot tubs, saunas, and chlorinated pools can dry out the skin and worsen keratosis pilaris symptoms. If you do choose to use these facilities, be sure to rinse off thoroughly afterwards and apply a moisturizer.
- Stay hydrated: Drinking plenty of water throughout the day can help to keep your skin hydrated from the inside out. Aim for at least 8 glasses of water per day, and more if you exercise or live in a dry climate.
- Manage stress: Stress can trigger or worsen skin conditions like keratosis pilaris. Practice stress-management techniques such as deep breathing, meditation, or yoga to help keep stress levels in check.
In addition to these tips, it’s important to protect your skin from sun damage. While sun exposure can temporarily improve the appearance of keratosis pilaris, UV rays can also dry out the skin and cause long-term damage.
Always wear a broad-spectrum sunscreen with an SPF of at least 30 when spending time outdoors, and reapply every 2 hours or after swimming or sweating.
The Emotional Impact of Keratosis Pilaris
While keratosis pilaris is a benign condition, it can still have a significant impact on a person’s self-esteem and body image.
Many individuals with keratosis pilaris feel self-conscious about the appearance of their skin, especially in social situations where the bumps may be visible, such as at the beach or pool.
It’s important to remember that keratosis pilaris is a very common condition, affecting up to 50 – 80% of adolescents and 40% of adults.
You are not alone in your struggles, and there is no reason to feel ashamed or embarrassed about your skin.
Practicing self-care and building self-confidence can go a long way in managing the emotional impact of keratosis pilaris. This may involve focusing on your positive attributes, surrounding yourself with supportive friends and family, and engaging in activities that make you feel good about yourself.

Embracing Your Skin: Managing Keratosis Pilaris with Confidence
Keratosis pilaris is a common, harmless skin condition caused by the buildup of keratin in the hair follicles. While it can be frustrating and emotionally challenging to deal with, there are many effective treatments and self-care strategies available to help manage its symptoms.
By incorporating gentle exfoliation, consistent moisturization, and lifestyle changes into your skincare routine, you can significantly improve the texture and appearance of your skin. It’s important to be patient and persistent, as it may take several weeks or months to see noticeable results.
If your keratosis pilaris symptoms are severe or not responding to self-care measures, don’t hesitate to consult with a dermatologist. They can provide personalized recommendations and prescription treatments to help you achieve the best possible results.
Remember, you are not defined by your skin condition. With the right tools, knowledge, and support, you can learn to manage your keratosis pilaris and live your life to the fullest.

Frequently Asked Questions About Keratosis Pilaris
What is keratosis pilaris and what causes it?
Where does keratosis pilaris commonly occur on the body?
What are the symptoms of keratosis pilaris?
- Small, rough, skin-colored or red bumps.
- Dry, sometimes itchy skin.
- Bumps that resemble pimples or have a plug in the center.
- Skin that feels like sandpaper to the touch.
Is there a cure for keratosis pilaris? Does it go away on its own?
What treatments are available for keratosis pilaris?
- Moisturizers containing exfoliating ingredients like lactic acid, glycolic acid, or urea.
- Topical retinoids to promote cell turnover.
- Laser treatments to reduce redness and improve skin texture.
- Microdermabrasion to physically exfoliate the skin.
How long does it take to see improvement with keratosis pilaris treatment?
Will keratosis pilaris return if treatment is discontinued?
Does keratosis pilaris get better or worse with age?
What aggravates keratosis pilaris?
- Dry skin.
- Cold weather.
- Having eczema or atopic dermatitis.
- Hormonal changes, such as during pregnancy.
When should I see a doctor about my keratosis pilaris?